Does Vitamin D-Deficiency
Result in Alzheimer’s & Other
Neurocognitive Disorders?
Evelyn
Smith (M. S. in Library Science, University of North Texas, 2012)
The body’s delicate; [this] tempest in my mind
Doth from my senses take all feeling else . . . .
King
Lear
III, iv, 13-14
Edited and Added to February 17, 2016
Medical Studies Linking Vitamin D
Deficiency with Alzheimer’s
On
August 6, 2014, the August issue of Neurology
published a groundbreaking longitudinal study that linked the risk of
developing Alzheimer’s and other dementias with low levels of vitamin D in the
blood. While correlation doesn’t equate
with causation, this research publicized the use of vitamin D supplements and
omega-3 fatty acid as possible means of delaying and/or preventing cognitive
decline. All of which also suggests
that older adults need to up their intake of vitamin D as a preventive measure
just as they need to get enough exercise, eat a healthy, balanced diet,
and maintain a support group of close friends.
For an earlier take on the general benefits of vitamin D, go to Shining the light on the benefits of vitamin D. (2013, March 7). STEM Library Science Blog. Retrieved from https://www.blogger.com/blogger.g?blogID=2149812825538872690#editor/target=post;postID=970504028190340250;onPublishedMenu=posts;onClosedMenu=posts;postNum=15;src=postname
___________
A Sampling of Bibliographic Sources on
Vitamin D Deficiency and Dementia
Researchers
obtained blood samples from 1, 658 ambulatory older adults between 1992-1993
and 1999 as part of a Cardiovascular Health Study, first obtaining serum 25-hydroxyvitamin D
concentration levels through liquid chromatography-tandemass spectrometry in
1992-1993 and then conducting a follow-up assessment in 1999 to determine if
the participants had developed Alzheimer’s or dementia in the intervening
years. They discovered that the 102 participants who had developed Alzheimer’s
were severely deficient in vitamin D compared with those who had healthy amounts of vitamin D3 in their blood. The research thus associated vitamin D
deficiency with a “substantially increased risk” of Alzheimer’s and other types
of dementia (Littlejohn, 2014, August 6, Abstract, para. 1-4).
An
online publicity post publicizes, summarizes, and enumerates the findings of
the August 2014 Neurology article:
After
collecting and analyzing blood samples for serum 25 (OH) D in a sample of
adults who were age 64 or older in 1992-1993, researchers over a mean follow-up
period of five to six years determined that the risk of Alzheimer’s was 60 percent
higher in those participants whose blood was severely lacking in vitamin D
[here the researchers round off the percentages]. Consequently, clinical trials are needed to
tell whether vitamin D supplements prevents Alzheimer’s in older adults. The
study, however, needs to be studied within the context of previous research
that also associates the risk of Mild Cognitive Impairment, late-onset
Alzheimer’s, and other types of dementia in older adults with low levels of vitamin D3
in the blood.
Annweiler, C., and Bequchet, O.
(2011). Vitamin D-mentia. Randomized clinical trials should be the
next step. Neuroepidemiology, 37 (3-4), pp. 249-55. doi:
10.1159/000334177. [Free full text]. Retrieved from
http://www.ncbi.nlm.nih.gov/pubmed/22156654
Since taking vitamin D supplements
might possibly stabilize Alzheimer's or prevent age-related cognitive
decline, Annweiler and Bequchet call for randomized, clinical trials
comparing the results of administering a vitamin D supplement and a
placebo and their effects on cognitive impairment and Alzheimer's.
Cross-sectional studies have associated Vitamin D intake from diet,
sun exposure, and supplements have strengthened the hypothesis that
Vitamin D preserves cognitive function, but they can't show the
empirical evidence that proves a cause and effect link (Annweiler, Abstract only, p. 249).
Annweiler C., Dursun E. and Féron F. et al. (2014, July 18). Vitamin D and cognition in older adults’: Updated international recommendations. Journal of Internal Medicine. [Abstract only]. doi: 10.1111/joim.12279. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/24995480
Hypovitaminosis D, or a deficiency in vitamin D, increases the risk of dementia in older adults, even though the testing for a lack of vitamin D shouldn’t be used as a diagnostic tool or bio-marker of Alzheimer’s at this time, according to researchers attending an international, invitational conference on “Vitamin D and Cognition in Older Adults”. Nevertheless, adults over age 65 should be regularly screened for Vitamin D deficiency (Annweiler, 2014, July 18, Abstract, para. 1-4).
Annweiler, C., Fantino, B., and
Schott, A. M., et al. (2012, July). Vitamin D insufficiency
and mild cognitive impaimentcross-sectional association. Euuropean
Journal of Neurology, 19 (7), pp.1023-29. doi:
10.1111/j.1468-1331.2012.03675.x. [Abstract only]. Retrieved from
http://www.ncbi.nlm.nih.gov/pubmed/22339714
After comparing community-dwelling,
cognitively healthy individuals with those with subjective memory
complaints, French researchers discovered that older women
complaining of memory loss were more likely to have lower
concentrations of low serum 25 hydroxyvitamin D in their blood
(Annweiler, 2012, July, Abstract, p. 1023).
Annweiler, C., Llewellyn, D., J., and
Beauchet, O. (2013). Low serum vitamin D concentrations in
Alzheimer's disease: A systematic review and meta-analysis. Journal
of Alzheimer's Disease: JAD, 33 (3), pp. 659-74. [Abstract only].
doi: 10.3233/JAD-2012-121432. Retrieved from
http://www.ncbi.nlm.nih.gov/pubmed/23042216
A Medline and PsycINFO search in May
2012 generated a meta-analysis that confirmed that adults diagnosed
with Alzheimer's had lower serum levels of vitamin D levels in their
blood that their matched controls (Annweiler, 2013, Abstract, p.
659).
Annweiler, C., Rolland, Y. and Schott,
A. M., et al. (2012, November). Higher vitamin D dietary
intake is associated with lower risk of Alzheimer's disease: A 7-year
follow-up. The Journals of Gerontology. Series A: Biological
Sciences and Medical Sciences, 67 (11), 1205-11. doi:
10.1093/gerona/gls107. [Abstract only]. Retrieved from
http://www.ncbi.nlm.nih.gov/pubmed/22503994
A Toulouse, France, cohort study
divided 498 community-dwelling women, aged 75 and younger, who were
free of vitamin D supplements, and measured their baseline vitamin D
intake based upon a self-reported food-frequency questionaire. Those
women with a lower baseline of Vitamin D intake were more likely to
have developed Alzheimer's seven years later. Conversely, those
women who reported a higher level of Vitamin D intake based on their
dietary choices were less likely to be diagnosed with Alzheimer's
(Annweiler, 2012, November, Abstract, p. 1205).
Assman, K. E., Touvier, M., and
Andreeva,V. A., et al. (2015, May 28). Midlife plasma vitamin
D concentrations and performance indifferent cognitive domains
assessed 13 years later. The British Journal of Nutrition,
113 (10), pp. 1628-37. [Abstract only]. Retrieved from
http://www.ncbi.nlm.nih.gov/pubmed/25864611
After measuring concentrations of
25-Hydroxyvitamin D in plasma samples in French adults, aged 40 to 60
years between 1994 and 1995 and then evaluating their cognitive
performance between 2007 to 2009, researchers discovered a positive
association between sufficient Vitamin D intake in midlife and
short-term working memory, although additional years of formal
education might also equip better educated adults with a cognitive
reserve (Assman, 2015, May 28, Abstract, p. 1628).
Annweiler
C., Dursun, E. and Féron F. et al.
(2014, July 18). Vitamin D and cognition
in older adults’: Updated
international recommendations. Journal of Internal Medicine. [Abstract
only]. doi: 10.1111/joim.12279.
Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/24995480
Hypovitaminosis
D,
or a deficiency in vitamin D, increases the risk of dementia in older adults,
even though the testing for a lack of vitamin D shouldn’t be used as a
diagnostic tool or bio-marker of Alzheimer’s at this time, according to
researchers attending an international, invitational conference on “Vitamin D
and Cognition in Older Adults”. Nevertheless, adults over age 65 should be
regularly screened for Vitamin D deficiency (Annweiler, 2014, July 18,
Abstract, para. 1-4).
Balion
C., Griffith, L. E., and Strifler L., et
al. (2012, September 25). Vitamin D,
cognition, and dementia: a systematic
review and meta-analysis. Neurology,
79 (13), pp. 1397-405. [Abstract]. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/23008220
After
searching five English-language databases up to August 2010, researchers found
37 studies that found that vitamin D exerted a positive effect in preventing
Alzheimer’s. Conversely, this survey connected
lower vitamin D levels with “poorer cognitive function” and a “higher risk of
AD” (Balion, 2012, September 25, Abstract, p. 1397).
Brouwer-Brolsma, E. M., and deGroot,
L.C. (2015, January). Vitamin D and cognition in older adults: An
update of recent findings. Current Opinion in Clinical Nutrition
and Metabolic Care, 18 (1), pp. 11-6). doi:
10.1097/MCO.0000000000000114. [Abstract only]. Retrieved from
http://www.ncbi.nlm.nih.gov/pubmed/25225898
Recent research posits that vitamin D
helps in the sending and creation of neurons as well as their
synaptogenesis, the clearing of amyloid plaque, and the prevention
of neuron death. Observational studies have also associated higher
serum levels of vitamin D with better cognitive performance, although
imaging studies and randomized trials are “scarce”
(Brouwer-Brolsma, 2015, January, Abstract, p. 11).
Dickens, A. P., Lang, I. A, and Laga,
K. M., et al. (2011, August). Vitamin D, cognitive
dysfunction and dementia in older adults. CNS Drugs, 25 (8),
pp. 629-39. doi: 10.2165/11593080-000000000-00000. [Abstract only].
Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/21790207
While medical science has long
associated insufficient vitamin D with osteoporosis and has recently
correlated low levels of vitamin D with cancer, heart disease,
stroke, and type-2 diabetes, recent research has associated
low levels of vitamin D with an increased risk of cognitive
dysfunction and Alzheimer's: For example, the risk of cognitive
decline was 60 percent higher in Italian males with severely
deficient vitamin D levels, and the risk of developing Alzheimer's
was 41 percent higher in American men with low levels of vitamin D (Dickens, 2011, August, Abstract, p. 629).
Dursun
E, Gezen-Ak D, & Yilmazer S. (2011). A novel perspective for Alzheimer's
disease: Vitamin D receptor
suppression by amyloid-β and preventing the amyloid-β induced alterations by
vitamin D in cortical neurons. Journal of
Alzheimer’s Disease, 23 (2), pp. 207-19. doi:
10.3233/JAD-2010-101377. [Abstract only]. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/24413618
While Amyloid-β (Aβ) (or the amino acids that form the amyloid plaques associated with Alzheimer’s) triggers gene mutations that result in the loss of the neurons
that transmit messages within the brain, vitamin D protects neurons in the
cerebral cortex by preventing cell
damage and cell death (Dursun, 2011, Abstract, p. 207).
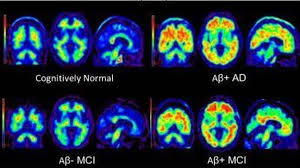 |
| Cognitively normal and brains filled with amyloid-beta plaque compared |
Fiala,
M. & Mizwicki, M. T. (2011). Neuroprotective and immune effects of active
forms of vitamin D3 and
docosahexaenoic acid in Alzheimer disease patients. Functional Foods in Health and Disease, 12, pp. 545-554. [Open
Access]. Retrieved from http://www.functionalfoodscenter.net/files/48097603.pdf
Because the skin of older adults absorbs less sunlight
than it did when they were younger, and/or they are less likely to send time in
the sun, many older adults get less vitamin D than they did when they were
younger, and they don’t eat enough fatty fish and fresh fruits and vegetables. These factors might make them more
susceptible to Alzheimer’s disease. Preventing Alzheimer’s disease therefore might in
part boil down to simple changes in diet: Avoiding simple carbohydrates, like sugar, and consuming more
complex carbohydrates, like green vegetables, whole grains, starches,
and lentils, avoiding saturated fat, and regularly including vitamin D, which
is mostly found in omega-3 fatty fish, in the diet. Vitamin D acts as a neuro-protective agent since it
clears out amyloid-beta plaque and inhibits the process of amyloid-precursor
protein, inflammatory toxics, and cell death. An increased consumption of vitamin D
and fish oil might prevent the degeneration of neurons in the outer brain (Fiala, 2011, Abstract, p. 545).
Gezen-Ak, D., Yılmazer, S., and Dursun, E. (2014). Why
vitamin D in Alzheimer's disease? The hypothesis. Journal
of Alzheimer’s Disease, 40 (2), pp. 257-69. doi: 10.3233/JAD-131970. [Abstract
only]. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/24413618
Researchers posit that vitamin D protects the
nervous system, and they suggest that disrupting vitamin D pathways mimics
amyloid pathology. Furthermore, they hypothesize that Alzheimer’s disease might
be the result of a long-time hormonal imbalance wherein there is a deficiency
in vitamin D (Gezen-Ak, 2014, Abstract, p. 257).
Gezen-Ak, D., Dursun, E., Yilmazer, S. (2012, December 19). Vitamin D inquiry in hippocampal neurons: consequences
of vitamin D-VDR pathway disruption on calcium channel and the vitamin D
requirement. Neurological Sciences,
34(8), pp. 1453-1458. doi: 10.1007/s10072-012-1268-6. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/23250517
The vitamin D receptor (VDR) and the enzymes
involved in activating the effects of vitamin D are most likely to affect the
brain’s hippocampus. Here amyloid beta (Aβ) pathology depletes VDR protein
depletion and disrupts vitamin D-VDR pathways.
Using rat embryos, researchers have determined that in older adults a
greater gene expression of 24OHase and VDR might call for a "higher
requirement of vitamin D" in the hippocampus to prevent cognitive decline (Gezen-Ak, 2012, December 19, Abstract, p. 1453).
Gezen-Ak, D., Dursun, E., & Bilgiç B, et al,.
(2012, October 16). Vitamin D receptor
gene haplotype is associated
with late-onset Alzheimer's disease. Tohoku
Journal of Experimental Medicine, 228 (3), 189-96. Retrieved from http://aja.sagepub.com/content/26/7/511.abstract
The continuing degeneration of the neurons in the
neo-cortex correlates with a high incidence of vitamin D deficiency, which also
causes depression and impaired cognitive performance in late-onset
Alzheimer’s. Vitamin D3 improves
cognitive function in patients with Alzheimer’s because of its active form of
vitamin D3 metabolite and its receptor in the central nervous system (Gezen-Ak, 2012, October 16, Abstract, p. 228).
Kapoor,
S. (2014, August). Influence of vitamin D consumption and levels
on the development of psychiatric disorders. Journal
of Clinical Psychopharmacology, 34 (4), pp. 538-539. doi: 10.1097/JCP.0000000000000169. Retrieved from http://journals.lww.com/psychopharmacology/Citation/2014/08000/Influence_of_Vitamin_D_Consumption_and_Levels_on.32.aspx
Getting enough vitamin D not only
prevents Alzheimer’s in the elderly, but an increased consumption of vitamin D
by mothers during pregnancy and in infants during the first year of life might
prevent schizophrenia in young adulthood most particularly in individuals of
sub-Saharan African descent (Kapoor, 2014, August Abstract, p. 538).
 |
| Getting enough vitamin E is essential for health throughout life. |
Llewellyn, D. J., Lang, I., and A. Lang, et al. (2010, July 12). Vitamin D and risk of cognitive decline in elderly persons. Archives of Internal Medicine, 170 (13), pp. 1135-1141. doi. 10.1001/archintermed.2010.173. [Open Access]. Retrieved from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4053858/
Researchers
have shown a correlation between low levels of vitamin D3
(25-hydroxyvitamin D) and an increased rise of cognitive decline in 858 Italian
adults aged 65 and older between 1988 and 2006. They first took blood
samples, testing for levels of vitamin D in the blood, and later asked
volunteers questions from the Mini-Mental State Examination (MMSE), and
interviewed them in follow-up assessments every three years (Llewellyn, 2010,
July 12, Abstract para. 2). This procedure associated low levels of vitamin D
with progressive cognitive decline particularly in older women (Llewellyn,
2010, July 12, Abstract, para. 4).
Llewellyn,
D. J., Lang, I. A., and Melzer, D. (2011, January). Vitamin D and cognitive impairment in the
elderly U.S. population. The Journals of Gerontology Series A:
Biological Sciences and Medical Sciences, 66S (1), pp. 59-65. [Open Access]. Retrieved from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3011960/
Since recent European research has associated
vitamin D deficiency with cognitive decline, this study investigated a possible
tie between the lack of vitamin D in blood samples and dementia in adults in
the United States aged 65 and older. A
nationally representative cross study of 3,325 non-institutionalized older
American showed significantly lower levels of serum hydroxyl-vitamin D in those
whose mental acuity testing disclosed increased cognitive impairment, shown by
impaired immediate and delayed memory, problems with orientation and a lower
attention span. These findings call for
the exploration of a possible causal relationship between vitamin D deficiency
and the onset of Alzheimer’s disease (Llewellyn, 2011, January, Abstract, para.
1-4).
Miller, J. W., Harvey, D. J., and Beckett, L. A., et al.
(2015, November). Vitamin D
status and rates of cognitive decline in a multiethnic cohort of older
adults. JAMA Neurology, 72(11),
pp. 1295-1303. doi.10.1001/jamameurol.2015.2115. [Abstract only]. Retrieve from http://archneur.jamanetwork.com/article.aspx?articleid=2436596
In a longitudinal, multi-ethnic study that took place
between February 2002 and August 2010, research associated low vitamin D status
with accelerated decline in episodic memory and executive functioning, most
particularly in African American and Hispanic older adults. However, Vitamin D status didn’t
significantly affect semantic memory or visuospatial ability.
Pogge,
E. (2010, July). Vitamin D and Alzheimer's
disease: is there a link? Consultant Pharmacist,
25 (7), pp. 440-50. doi: 10.4140/TCP.n.2010.440. [Abstract only]. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/20601349
After entering the key words vitamin D, Alzheimer
disease, and Vitamin D in the Medline/ PubMed database for sources published
between January 1950 and January 2010 and the ISI Web of Science database for
articles published between January 1900 and January 2010 as well as reviewing
The Cochrane Library and clinical trials.gov to identify unpublished research,
Pogge determined that not only is vitamin D deficiency a widespread and
long-standing problem in the elderly, but that researchers have recently linked
it with dementia, and most particularly Alzheimer’s disease. Hence, Pogge calls
on further trials with a longer follow-up period to determine if a cause and
effect relationship exists between a lack of vitamin D in the blood and a
diagnosis of Alzheimer’s (Pogge, 2010, July, Abstract, p. 440).
Schlögl,
Mathias & Holick, Michael F. (2014).
Vitamin D and neurocognitive function. Clinical
Interventions in Aging, 9, pp. 559-588. [Open Access]. Retrieved from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3979692/
Recent emerging evidence has not only
linked vitamin D deficiency with calcium-depleted bones and osteoporosis, but it
has also correlated it with Mild Cognitive Impairment and late-onset
Alzheimer’s. An increasing proportion of the elderly in developed countries
with low levels of vitamin D in the blood, in turn, enhances the importance of
these findings. A lack of vitamin D in
the diet along with a decreased inability for the skin to synthesize sunlight
into vitamin D as individuals grow older results in this insufficiency (Schlögl,
2014, Abstract, p. 559).
Shah,
I., Petroczi, A., & Tabet, N. (2012, November 9). Low 25OH Vitamin D2
levels found in untreated Alzheimer’s patients,
compared to Acetylcholinesterase inhibitor treated and controls. Current Alzheimer Research, 9 (9), pp.1069-1076. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/22876849\
This study contrasts the levels of 25-hydroxyvitamin
D (25-OH), or calcidiol, in
the blood of Alzheimer’s patients treated with acetylcholinesterase inhibitors
as well as those Alzheimer’s patients not treated with donepezil, rivastigmine
or galantamine, and a control group that didn’t show any signs of cognitive impairment The levels of 25-OH as well as 1,25-dihydroxyvitamin D, or
calcitrol, were significantly lower in the untreated group when compared to
those patients prescribed acetylcholinesterase inhibitors and their cognitively
healthy controls. The reader will also find that browsing the
interpretation of medical references on vitamin D and cognitive decline in
popular, non-medical sources particularly helpful (Shah, 2012, November 9, Abstract, p. 1069).
These comparisons also point out the
occasional over simplification of complex medical issues, although some more
insightful articles provide hyperlinks to PubMed abstracts and Open Access
sources if their audience wants to verify or further explore a particular
study’s findings. A comparison of these studies is important since it
emphasizes that maintaining a high level of vitamin D is just one of the
tactics that older adults might use to delay or prevent the onset of dementia,
including getting enough physical exercise, not succumbing to depression, and
striving for happiness with the help of a caring support group of friends. Western medicine, however, often forgets that a form
of vitamin D3 is found in curcumin (turmeric), a key ingredient
found in curry powder(Shah, 2012, November 9, Abstract, p. 1069).
See also:
Mishra,
S. and Palanivelu. (2008, January-March).
The effect of curcumin (turmeric) on Alzheimer’s
disease. Annals of Indian Academy on Neurology, 11 (1), pp. 13-19. Retrieved from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2781139/
Indian medicine has extensively studied curcumin (turmeric), for treatment of dementia and brain injury. This antioxidant and anti-inflammatory herb
used in curry powder improves the cognitive function of Alzheimer’s patients
since it shrinks amyloid beta plaques, delays the breaking down of neurons,
chelates heavy metal, and even improves memory (Mishra, 2008, January-March,
Abstract, p. 13).
Type
1 Vitamin D3 receptors block amyloid-beta plaque from forming while
bisdemethoxy-curcumin (BCC) promotes the engulfing, or phagocytosis, of amyloid
beta protein, by type 1 macrophages, or immune cells (Mizwicki, 2012, Abstract, p. 51).
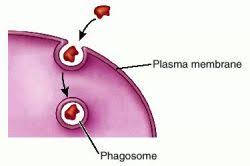 |
Phagocytosis
____________ |
Popular Resources Connecting Vitamin D
Deficiency with Alzheimer’s & Dementia
 |
| Vitamin D flushes out amyloid-beta plaques from the brain. |
Vitamin D deficiency is common in
older adults because of the skin’s reduced ability to synthesize sunlight into
vitamin D. Research associates higher
levels of vitamin D with a reduced risk of Alzheimer’s. Older adults may therefore need to supplement
their diet with 800 IU of vitamin D daily (as compared to a recommended adult
dose of 400 IU), but they should check with their physician first (Alzheimer’s
Prevention, n. d., para. 6). However,
taking vitamin D supplements is just one of the steps to prevent Alzheimer’s:
Keeping physically active since research shows a link between cardio-respiratory fitness and a healthy hippocampus, the area of the brain responsible for memory (Alzheimer’s Prevention, n. d., para. 1).
Exercising the brain and keeping socially active because this strengthens the links between brain cells (Alzheimer’s Prevention, n. d., para. 2).Eating healthy, unsaturated, un-hydrogenated fats to ensure cardiovascular health as well as including in the diet plenty of green vegetables, like spinach and beans, that are rich in folic acid, and consuming fortified cereals, meat, and liver for vitamin B12 (Alzheimer’s Prevention, n. d., para. 3).
Getting enough vitamin E and C in the diet is important because this reduces the risk Alzheimer’s by controlling the damage produced by free radicals (Alzheimer’s Prevention, n. d., para. 5). Consumers can find Vitamin E in meat, poultry, eggs, fruits, and vegetables, and wheat germ, and they may also take it as a supplement (Vitamin E, 2009, Web M.D., para. 1).
They can also get enough vitamin C by drinking
one glass of [red] wine or beer daily whereupon resveratrol will also decrease
levels of amyloid plaque (Alzheimer’s Prevention, n. d., para. 6).
See
also:
Web M.D. tells the reader almost everything h or she needs to know about Vitamin E.
 |
| Vitamin E is found in foods and available as a supplement. |
Li,
D., Gong, Q., & Dong, H, et al.
(2012). Resveratrol, a neuro-protective
supplement for Alzheimer's disease. Current Pharmaceutical Design, 18 (1), pp. 27-33. [Abstract only]. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/22211686
In 1992 research showed that resveratrol proved
beneficial in preventing coronary heart disease. Subsequent research also indicates that it
may be useful in treating and deferring cardiovascular disease, certain
cancers, pain, inflammation, tissue injury, and Alzheimer’s disease since it
clears amyloid beta peptides and reduces neuron damage. Resverastrol is found
not only in grapes, but it is also in berries and peanuts (Li, 2012, Abstract, p. 27).
Note: Resveratrol deserves its own bibliography, so
keep checking back to this STEM Library
Science blog!
------------
Sufficiently encouraging results exist in longitudinal studies linking lower
concentrations of vitamin D to Alzheimer’s to warrant further clinical trials
to determine if a cause and effect relationship exists between low
concentrations of vitamin D in the blood and the incidence of Alzheimer’s,
according to Cynthia Balion, a biochemist
at McMaster University in Hamilton, Ontario, Canada. Balion and her colleagues searched Medline,
Embase, Amed, PsychINFO, and the Cochrane Central databases for diagnostic
criteria and came up with 37 studies showing a link between Alzheimer’s and
lower levels of vitamin D, of which 30 included only older participants
(Anderson, 2012, September, p. 1).
Although Balion stressed a need for standardized
methods of measuring 25OH Vitamin D3, a second meta-analysis
revealed that older adults with higher than average Mini-Mental State
Examination (MMSE) scores also had higher concentration of vitamin D3 in
their blood. This implies
that vitamin D acts as a meurosteroid (Anderson, 2012, September, p. 2). Balion therefore advises that physicians
should recommend vitamin D supplements for patients who do not have enough vitamin
D in their blood, even though results of such blood tests are influenced by latitude,
the time of year, and ethnicity (Anderson, 2012, September, p. 3).
A University of Exeter follow-up study
that controled for dementia risk factors like age, educational level,
gender, BMI, smoking, alcohol use, diabetes, and hypertension in a
sample size of 1,658 cognitively and physically healthy men and women
with the average age of 73 at the start of the original study found
that low levels of vitamin D in the blood increased the risk of
Alzheimer's and other types of dementia: Compared with those older adults
with 50 or more nanomoles per liter of vitamin D in their blood,
those with levels of 25 to 50 nanomoles per liter had a 53 percent
increased risk of dementia and a 69 percent increased risk for
Alzheimer's while those with readings of 25 or less of vitamin D in a
liter of blood were twice as likely to develop Alzheimer's (Bakalar,
2014, August 14, para. 1-3). Senior Lecturer Iain A. Lang at the
University of Exeter, however, cautioned that these “exciting and
suggestive” results were only “observational” (Bakalar, 2014,
August 14, para. 5).
Chan,
Amanda L. (2012, March 8). Vitamin D and
Alzheimer’s: Study shows how the nutrient
can help the brain ward
off any amyloid plaques. Healthy
Living. Huffington Post. Retrieved
from http://www.huffingtonpost.com/2012/03/08/vitamin-d-alzheimers-amyloid-beta-plaque-protein_n_1326952.html
A recent released study shows that
vitamin D may clear amyloid plaque by activating certain genes that signal cell
networks to “ramp up” the immune system (Chan, 2012, March 8, para. 1 & 2). Taking blood samples from individuals diagnosed with Alzheimer’s and
cognitively healthy participants, scientists separated the immune cells
responsible for unblocking amyloid beta protein (Chan, 2012, March 8, para.
4). A similar 2009 study found that
vitamin D3 coupled with the spice curcumin worked together to unclog
amyloid beta plaque while 2010 research demonstrated that lower levels of
vitamin coincide with a higher risk of cognitive decline (Chan, 2012, March 8,
para. 5-6).
Dockterman,
Eliana. (2014, August 7). Low vitamin D
increases risk for dementia and Alzheimer’s study
says. Time. Retrieved from http://time.com/3089339/study-research-vitamin-d-deficiency-dementia-alzheimers/
Research
shows a correlation not a causal link that exists between
low levels of vitamin D and Alzheimer’s and other dementias. Nevertheless, a study published August 6,
2014 in Neurology and summarized
above hypothesizes that older adults with moderate to severe vitamin D
deficiency are “significantly more likely” to develop dementia in (Dockterman,
2014, August 7, para. 1-2 & 4).
This six-year, longitudinal study found that is a
sample size of 1,658 Americans age 65 and older, participants who were
moderately deficient in vitamin D were 53 percent more likely to be diagnosed
with any form of dementia while those severely deficient were 125 percent more
likely to develop Alzheimer’s (Dockterman, 2014, August 7 para. 3). The project’s leader, David Llewellyn of the
University of Exeter Medical School, emphasized that clinical tests still need
to establish whether or eating oily fish or taking vitamin D supplements might
best prevent or delay Alzheimer’s and other dementias (Dockterman, 2014, August
7, para. 5).
University of Exeter Medical School
researchers correlated dementia with the severity of Vitamin D
deficiency when they revisited the U.S. Cardiovascular Health Study
of 1,600 adults over age 65 that took place between 1992-1993 and
1999 and compared the blood samples that analyzed Vitamin D content
in blood plasma with the participants mental acuity six or more years
later. However, the study's findings weren't strong enoung to
recommend that older adults take Vitamin D supplements, for their
analysis didn't prove a cause and effect link. Thus, researchers as
of yet don't know whether upping one's dietary intake of Vitamin D or
getting more sun exposure would help (Doheny, 2014, August 11, para.
1-5 & 8). Nevertheless, this comparative study does build on
evidence that Vitamin D maintains strong bones, moderates cell
growth, controls immune functions, and lessens inflammation (Doheny,
2014, August 11, para. 7).
Researchers discovered that low levels
of Vitamin D corresponded with a 1.7 great risk of developing
dementia while severely low levels of Vitamin D increased the changes
of developing Alzheimer's 2.2 times (Doheny, 2014, August 11, para.
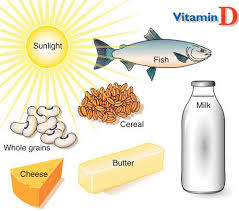
10). While sun exposure provides the body with Vitamin D, it is also
found in fatty fish, like salmon, tuna, and mackerel, as well as in
milk, eggs, and cheese. Experts nevertheless disagree about the
optimal level of Vitamin D in the blood, but they do agree that the
risk of dementia significantly increases when it falls below 50
nanometers per liter (Doheny, 2014, August 11, para. 9 & 11).
Fenner,
James. (2013, December 4). Vitamin D deficiency linked to brain damage, says
study. Guardian
Liberty Voice.
Retrieved from http://guardianlv.com/2013/12/low-vitamin-d-levels-linked-to-brain-damage-says-study/
Fenner summarizes a collection of studies linking
vitamin D deficiency with brain damage, including a contemporize University of
Kentucky study published in Freeradical
Biology and Medicine (2013,
December 4, para. 1). Vitamin D is a fat
soluble hormone found in fatty fish, cheese, egg yolks, and fortified mil, and
cereal, although the body soaks up most of its store of vitamin D when the
sun’s rays strike the skin (Fenner, 2013, December 4, para. 2).
Vitamin D performs
multiple functions:
- Vitamin D helps the body absorb and maintain calcium levels that build strong bones;
- It regulates genes that control cell division and death;
- It inhibits inflammation and neuromuscular damage;
- It also imparts immunity from various diseases.
(Fenner, 2013, December 4, para.
3)
Additionally, vitamin D may also protect the brain
from free radical damage, according to a series of trials wherein researchers
administered middle-age male-rats for four-or-five-months low concentrations of
vitamin D versus merely adequate and abundant amounts of vitamin D. The rats
given the most Vitamin D excelled at cognitive tests while those given a diet
deficient in vitamin D didn’t perform as well (Fenner, 2013, December 4, para.
4-8). Poverty, latitudes with little or
no sunlight, working indoors for long periods of time, sedentary life styles,
and age may all aggravate vitamin D deficiency (Fenner, 2013, December 4, para.
9).
Previous studies have linked vitamin D deficiency,
or hypovitaminosis, with a higher incidence of Alzheimer’s, and most recently they
have correlated a lower level of vitamin D in the blood of Alzheimer’s patients
when compared to their cognitively healthy peers (Fenner, 2013, December 4,
para. 10). A 2011 Lu’o’ng and Nguyễn
study also found that low levels of Vitamin D could set off “mood problems and
cognitive impairment” (Fenner, 2013, December 4, para. 11).
Other studies have established a link between
vitamin D deficiency and certain cancers, cardio-vascular conditions,
osteoporosis, and rickets (Fenner, 2013, December 4, para. 12) Fenner thus recommends a diet rich in vitamin
D and getting at least 10 to 15 minutes of direct sunlight daily. However,
patients should consult their physician to check for vitamin D levels and ask
him or her about taking supplements (Fenner, 2013, December 4, para. 13).
|
|
| A link exists between depression, low-levels of vitamin D, and Alzheimer's. |
Two articles published in the August 6, 2014 issue
of Neurology have established a
connection between a deficiency in vitamin D and Alzheimer’s as well as an
association between depression and cognitive decline. However, the study that has received the most
publicity, Littlejohns, Henley, and Lang’s, et
al, “Vitamin D and the Risk of Dementia and Alzheimer Disease”, which is
summarizes above, theorizes that older adults that don’t get enough vitamin D
double their risk of Alzheimer’s (Fischer, 2014, August 6, para. 1-2). The leader of this team of researchers, David J. Llewellyn of the University of Exeter explains that the researchers found the association ended up "twice as long as anticipated" (Fischer, 2014, August 6, para. 4).
The
leader of this team of researchers, David J. Llewellyn of the
University of Exeter, explains, “We expected to find an association
between low vitamin D levels and the risk of dementia and Alzheimer's
disease, but the results were surprising — we actually found that
the association was twice as strong as we anticipated” (Fischer,
2014, August 6, para. 4).
Moreover,
these results did not vary even when researchers adjusted them for
other risk factors, such as smoking, alcohol consumption and level of
formal education (Fischer, 2014, August 6, para. 6). Llewellyn,
however, cautioned that further studies would need to reveal whether
vitamin D supplements or eating foods high in vitatim D would best
delay or prevent dementia (Fischer, 2014, August 6, para. 7). He also
emphasized that a correlation between low levels of vitamin D with
the presence of Alzheimer's does not necessarily prove that a vitamin
D deficiency causes cognitive decline (Fischer, 2014, August 6, para.
8).
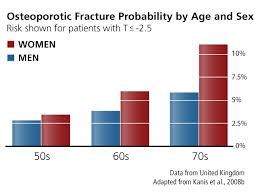 |
| Osteoporosis is another reason to get enough Vitamin C. |
Llewellyn nevertheless acknowledges that past trails
have shown that boosting vitamin D has proven effective in treating other
health problems; for example, increasing the intake of vitamin D prevents bone
fractures. Accordingly, the elderly
should eat a balanced diet that includes regularly eating oily fish as well as
maintain an active lifestyle, and going outdoors regularly for moderately
intensive exercise (Fischer, 2014, August 6, para. 9-10).
In a related Rush University Medical Center study,
also published in the August 2014 issue of Neurology,
Wilson, Capuano, and Boyle’s, “Clinical-pathologic Study of Depressive Symptoms
and Cognitive Decline in Old Age”, researchers
showed that the elderly who suffer from depression have a greater risk of
developing Alzheimer’s in a study that followed 1,764 volunteers for eight
years. Those who were eventually
diagnosed with dementia or mild cognitive impairment were more likely to be
depressed before their diagnosis of cognitive decline (Fischer, 2014, August 6,
para. 11-12).
Consequently, since these findings suggest that
depression is a risk factor for dementia, if depression and stress can be prevented
or successfully treated, medical science may be able to help the elderly keep
their memories and ability to think and reason, according to Rush Alzheimer’s
Disease Center neuropsychologist, Robert S. Wilson (Fischer, 2014, August 6,
para. 13).
Fischer also provides a
hyperlink for the study that connects depression and dementia:
___________
Glatter,
Robert. (2014, August 7). Dementia risk
and vitamin D levels: Is there a connection? Forbes. Retrieved from http://www.forbes.com/sites/robertglatter/2014/08/07/dementia-risk-and-vitamin-d-levels-is-there-a-connection/
Vitamin D deficiency may double the risk of cognitive decline and loss of memory, according to a study published online in Neurology on August 6, 2014 (Glatter, 2014, August 7, para. 13). After evaluating levels of vitamin D in the bloodstream of 1,658 healthy adults over age 65, researchers expected to find a link between low levels of vitamin D and the ability to think, remember, and reason, but the association proved twice as strong as they anticipated (Glatter, 2014, August 7, para. 4-5).
Vitamin D deficiency may double the risk of
cognitive decline and loss of memory, according to a study published online in
Neurology on August 6, 2014 (Glatter, 2014, August 7, para. 13).
After
evaluating levels of bloodstream in the bloodstream of 1,658 healthy adult
volunteers over age 65, researchers expected to find a link between low levels
of vitamin D and the ability to think, remember, and reason, but the
association proved twice as strong as they had anticipated (Glatter, 2014,
August 7, para. 4-5). Thus, individuals with comparatively low levels of
vitamin D were 53 percent more likely to develop memory and reasoning problems
while those with a “significant deficiency” stood a 125 percent better chance
of developing dementia compared to individuals with normal levels of vitamin D
(Glatter, 2014, August 7, para. 6).
Indeed, those individuals whose blood contained low
levels of vitamin D had a 70 percent greater risk of developing Alzheimer’s
while those with the severest deficiency in vitamin D increased their chances
of being diagnosed with Alzheimer’s by 120 percent even when researchers
controlled for other risk factors (Glatter, 2014, August 7, para. 7-8).
Further clinical trials might establish whether
eating oily fish or taking vitamin D supplements might best prevent or delay
Alzheimer’s, although the study doesn’t actually show that low levels of
vitamin D cause Alzheimer’s or other dementias (Glatter, 2014, August 7, para.
9-10). This means that a multifaceted approach to preventing Alzheimer’s is
necessary since diet, lifestyle, and genetic factors might all influence its
development. Even so, “good levels of
vitamin D” might help prevent the accumulation of amyloid plaque (Glatter,
2014, August 7, para. 11-12).
 |
| Two weekly servings of omega 3 fatty fish builds-up vitamin D levels. |
A pilot study published in the Journal of Alzheimer’s Disease, University
of California, Los Angeles, has announced that researchers have discovered the key gene that lies
behind vitamin D3 and omega-3’s ability to rid the brain of the amyloid plaque associated with
Alzheimer’s, Cyactiv, a blue antioxidant that
gives off a “healthy inflammation response” (Gray, 2013, February 12,
para. 1-7). Additionally, they have established that individuals with
Alzheimer’s have a different inflammatory gene than healthy controls (Gray,
2013, February 12, para. 9).
Drawing blood from both individuals
diagnosed with Alzheimer’s and cognitive-healthy older adults, researchers have
also isolated critical immune cells, called macrophages, after incubating the
immune cells overnight with amyloid-beta and then adding either an active form
of vitamin D3 or omega 3 fatty acid whereupon they determined the
effect these substances had on inflammation and amyloid-beta absorption. Both vitamin D3 and omega-3 fatty
acid improved the ability of the immune cells to break down amyloid beta and
inhibit cell death (Gray, 2013, February 12, para. 12-13). These findings might indicate that future
Alzheimer’s treatment might need to balance vitamin D supplements and the
consumption of omega 3 fatty acid, although a larger sampling size and clinical
trials is necessary to confirm these findings (Gray, 2013, February 12,
para. 16-18).
An international team of researchers
led by David J. Llewellyn of the University of Exeter Medical School has
determined that adults over age 65 who are evenly moderately deficient in
vitamin D stand a 53 percent greater risk of dementia while those with a severe
vitamin D deficiency raise their risk of developing Alzheimer’s 125 percent. Furthermore, those found to be moderately
deficient in vitamin D are 69 percent more likely to develop Alzheimer’s while
those with the lowest levels of vitamin D in their blood are 122 percent more
likely to do so (Kinkle, 2014, August 6, para. 2). The risk of dementia rises for levels of
vitamin D in the blood below 25 nanomoles per meter while vitamin D levels
above 50 nanomoles signify a sufficient level of vitamin D to maintain cognitive
health (Kinkle, 2014, August 6, para. 3).
While the researchers acknowledge
that dementia might alter behavior or diet in a way that might contribute to
vitamin D deficiency, they suggest this is unlikely (Kinkle, 2014, August 6,
para. 4). Even so, they admit that
further study needs to determine whether consuming oily fish or taking vitamin
D supplement might best prevent Alzheimer’s. Research, however, already suggests
that vitamin D might regulate calcium levels in brain cells (Kinkle, 2014,
August 6, para.5- 6). Vitamin D helps
the body use calcium when skin is exposed to sunlight. Experiments also show
that vitamin D might help rid brain cells of beta-amyloid plaque, breaking down
and carrying it away Kinkle, 2014, August 6, para. 9-10).
“The most robust
study of its kind ever conducted” published in the August 6, 2014 issue of Neurology has documented that older
adults who are severely deficient in vitamin D are twice as likely to develop
Alzheimer’s and other dementias (Pash, August 6, para. 1-2 & 5). Studying older Americans who took
part in the Cardiovascular Health Study, an international team of researchers
found that older adults moderately deficient in vitamin D had a 53 percent
chance of developing dementia of any kind, but the severely deficient in
vitamin D raised their risk 125 percent.
Those moderately deficient in vitamin D raised their risk of developing
Alzheimer’s 69 percent while those severely deficient in vitamin D had a 122
percent greater risk of eventually being diagnosed with Alzheimer’s (Pash,
2014, August 6, para. 3). Suffering from depression only adds to the risk of developing Alzheimer's since previous researchers have established
that individuals with low levels of vitamin D are more likely to develop mental
illnesses (Pash, 2014, August 6, para. 13).
The exposure of skin to sunlight produces vitamin D, which is also found
in oily fish and supplements, but older skin is less efficient than youthful
skin in converting sunlight to vitamin D (Pash, 2014, August 6, para. 14-15).
Vitamin D3 may turn on
certain genes to jump start the immune system to flush out the amyloid beta
plaques that form in the cerebral cortex of Alzheimer’s patients (Pederson,
2012, March 9, para.1-2). Prior
research shows that these immune cells respond favorably to vitamin D3
and curcumin, a turmeric spice; however, this particular study clarifies the
mechanism involved in this action by taking blood samples from Alzheimer’s
patients and healthy controls and then isolating their macrophages, or immune
cells, incubating them with amyloid beta amino acids and then introducing an
active form of vitamin D3 to see whether it absorbed the amyloid
beta peptides (Pederson, 2012, March 9, para. 2 & 4-5).
Apparently, two types of macrophages
exist:
- Type 1 clears amyloid beta amino acids after researchers introduce a solution of vitamin D3 and curcuminoids, a synthetic form of curcumin.
- Type 2 immune cells, however, are found in vitamin D3 alone.
In both types of macrophages, vitamin D3
opens a specific chloride channel (CLC3) that clears out amyloid beta peptides
(Pederson 2012, March 9, para. 6-7 & 9). Thus, the vitamin D3
found in Omega 3 fatty fish and in turmeric (or curcumin), which is an
ingredient in curry recipes, may help clear out amyloid plaques (Pederson,
2012, March 9, para. 8). Some authorities recommend taking Vitamin D and curcumin together since Vitamin D boosts curcumin's effectiveness.
 |
| Turmeric is a common ingredient in curry recipes. |
Indians
in their 70s are four times less likely to have Alzheimer’s than their
American counterparts are, and curry dishes, made with turmeric (curcumin) may contribute
to their mental health (Rodriguez-Paez, 2011, para. 2-5). The curcumin keeps
amyloid beta molecules from clumping together and disrupts them once they form.
Curcumin, a strong antioxidant, also reduces the amount of free radicals that
destroy brain neurons, and it removes heavy metals from the blood stream (Rodriguez-Paez,
2011, para. 10-11).
Turmeric (curcumin), the primary spice found in
curry, is also widely used as an Indian folk remedy to treat a wide variety of
ailments since it is thought to decrease swelling or inflammation (WebMD, 2014, para. 1-3 & 7).
____________
Pettersen, J. A. (2015, December 27).
Vitamin D and executive functioning. Are higher levels better?
Journal of Clinical and Experimental Neuropsychology, pp.
1-11. [E-pub ahead of print]. [Abstract only]. Retrieved from
http://www.ncbi.nlm.nih.gov/pubmed/26708262
In a study of 142 healthy adults,
research found that those with “supra-therapeutic levels” of
Vitamin D in their blood performed “significantly better" on verbal
fluency tests (Pettersen, 2015, December 27, Abstract, p. 1).
Pettersen, J. A., Fontes, S., and Duke,
C. L. (2014, July). The effects of Vitamin D insuficiecy and
seasonal decrease in cognition. The Canadian Journal of
Neurological Sciences, 41 (4), pp. 459-69. [Abstract only].
Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/24878470
After testing the working memory of 32
healthy adults and assessing the levels of Vitamin D in their blood
in both the summer and winter, they found that while 46 percent of
those with low Vitamin D performed poorly on memory tests in the
summer, in the winter, 63 percent had insufficient levels of Vitamin D
in their blood, and their memory skills had also declined. Thus,
researchers concluded that adults need to maintain their vitamin D
levels year round (Pettersen, 2014, July, Abstract, p. 459).
Philip,
John. (2013, October 24). Little known
form of vitamin D holds key to Alzheimer’s disease prevention. Natural News. Retrieved from http://www.naturalnews.com/042632_vitamin_d3_alzheimers_prevention_prohormone.html#
Researchers are finding that the same lifestyle
changes that thwart heart disease also prevent Alzheimer’s (Philip, 2013,
October 24, para. 1). In recent years,
researchers have verified that turmeric, or curcumin, resveratrol, and omega-3
fatty acids as well as vitamin D “retard or significantly delay” Alzheimer’s
(Philip, 2013, October 24, para.2)
In a study published in the November 9, 2012 issue
of Current Alzheimer Research, “Low 25OH
Vitamin D2 Levels Found in Untreated Alzheimer’s Patients, Compared
to Acetylcholinesterase-inhibitor Treated and Controls”, researchers examined blood samples of Alzheimer’s patients and healthy controls
and discovered that those diagnosed with Alzheimer’s had low cellular and circulatory stores of vitamin D (Philip, 2013, October 24, para. 3).
Lead researcher Declan Naughton explains that in older
adults diagnosed with Alzheimer’s vitamin D was “either nonexistent or in such
low qualities that it couldn’t be measured” (Philip, 2013, October 24, para.
4). Medical science has already determined that vitamin D lowers the
risk of cancer, cardio-vascular disease, stroke, and diabetes (Philip, 2013,
October 24, para. 5).
Senior adults with low levels of vitamin D in their blood are four times more likely to experience cognitive decline as their peers blessed with adequate levels of vitamin D, according to a study led by David Llewellyn, a neuropsychologist at the University of Exeter, who presented their findings at the Alzheimer’s Association International Conference. Llewellyn’s research-team analyzed 3,326 adults age 65 and older and determined that an adverse relationship existed between low levels of vitamin D and impaired thinking skills. Those participants with moderately low
levels of vitamin D were 42 percent more likely to perform poorly on memory and
mental acuity tests while those blood was “severely deficient” in vitamin D
were 400 percent more likely to flunk their Mini-Mental State Examination (Simon,
2012, July 13, para. 3). Most older adults in the United
States have low levels of vitamin D in their blood perhaps because the skin
becomes less effective in turning sunlight into vitamin D (Simon, 2012, July
13, para. 4-5). Researchers also hypothesize that vitamin D might protect the
blood supply to the brain as well as clear toxins, and break down amyloid-beta plaque (Simon, 2012, July 13, para. 6-7).
Soni, M., Kis, K., and Lang, I. A., et
al. (2012). Vitamin D and cognitive function. Scandinavian
Journal of Clinical and Laboratory Investigation. Supplemetum,
243, pp. 79-82. doi: 10.3109/00365513.2012.681969. [Abstract only].
Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/22536767
Cognitive decline and dementia need to
be added to the long list of conditions associated with lower levels
of Vitamin D, including osteoporosis, heart disease, stroke, cancer,
and type-2 diabetes. Vitamin D receptors are widespread in the
brain, and the active form of Vitamin D may clear beta-amyloid
plaques. European and United States studies also have associated low
levels of Vitamin D with an increased risk of Vitamin D—up to four
times greater in severely deficient Vitamin D older adults (Soni,
2012, Abstract, p. 79).
___________
Natural & Supplemental Sources
of Vitamin D3
Most Americans are vitamin D
deprived, even though every tissue in the body has receptors for the sunshine
vitamin. Consequently, vitamin D
deficiency raises the risk of colon, breast, and prostate cancer, high blood
pressure, cardiovascular disease, osteoarthritis, multiple sclerosis, and
rheumatoid arthritis (Brody, 2010, July 26, para. 1-3)—not to mention
Alzheimer’s, which Brody does not list in this catalogue of diseases brought on
by a modern lifestyle (Brody, 2010, July 26, para. 4). Brody, however, simplifies the
process of how sun-exposed skin turns into 25-hydroxyvitamin D3 in
the liver and 1,25 vitamin D , or vitamin D hormone, in the kidneys (Brody,
2010, July 26, para. 5). She also suggests that for maximum
bone density, the vitamin D3 found in blood samples should reach 40
nanograms per millimeter or more, although mitochondria Eve and Y-chromosomal
Adam’s blood probably had 50 nanograms per millimeter. However, not enough sun
exposure because of sunscreen and protective covering and perhaps not eating
enough fatty fish, like salmon and tuna, ensures that most individuals have lower
levels of vitamin D3 (Brody, 2010, July 26, para. 7-9).
Most
European Americans average 18 to 22 nanograms of vitamin D3
per
millimeter of blood while African Americans average between 13 to 15
nanograms of vitamin D3
per
millimeter of blood (Brody, 2010, July 26, para. 10).
The Northern United States has
higher rates of cancer than the South most probably because of reduced sun
exposure just as African Americans experience higher rates of high blood
pressure, heart disease, and prostate cancer since they have darker skin than
white Americans. Similarly, the rise of
Type 1 diabetes may stem from overly protecting young children from sun
exposure (Brody, 2010, July 26, para. 12).
Current medical practice recommends
an intake of at least 200 IU of vitamin
D3 daily up to age 50 and 400 I.U. of vitamin D3 a day
from age 50 to 70, so older adults and pregnant and lactating mothers need to
take a vitamin D supplement (Brody, 2010, July 26, para. 14). When the body
acquires vitamin D through sunlight, it has a built-in cut off, so it doesn’t
absorb too much vitamin D. Individuals
really deprived of vitamin D can also stand comparatively high doses (Brody,
2010, July 26, para. 16-18), but it is best to consult a physician before self-medicating.
According
to findings published in JAMA Internal
Medicine, 75 percent of all American teens and adults are deficient in
vitamin D.
Ginde,
A. A., Liu, M. C., & Camargo, C.C. (2009, March 23). Demographic differences and trends of Vitamin D
insufficiency in the US population, 1988-2004. JAMA Internal Medicine,
169 (6), pp. 623-632. doi: 10.1001/archinternmed.2008.604. Retrieved from http://www.scientificamerican.com/article/vitamin-d-deficiency-united-states/
Just 23 percent of the blood samples taken in this
survey had 30 nanograms per millimeter or more of vitamin D, and only 3 percent
of African Americans did so (Ginde, 2009,March 23, para. 2-3). Medical science has long linked vitamin D
insufficiency with osteoporosis and rickets, but recent research has determined
that it also correlates with heart diseases, diabetes, and cancer (Ginde, 2009,
March 23, para. 4). Skeptics, however, in part account for this drop in
vitamin D levels by noting that blood tests measure the amount of vitamin D in
the blood differently than they use to do (Lite, 2009, March 24, para.
6-7). Even so, Ginde, who insists the
study is reliable, blames this drop in vitamin D to an over-reaction to skin
cancer campaigns, and he even goes so far as to suggest that African Americans
take double the amount of vitamin D supplements recommended for whites (2009, March 23, para. 10).
The skin synthesizes vitamin D that
it takes from the sun, but the vitamin is found in lesser amounts in some foods,
or it can be taken as a supplement (Robin, 2014, para. 1). Vitamin D2, which comes from
plants, and vitamin D3 supplements are available, but authorities
believe the body absorbs vitamin D3 more efficiently. Spending from 5 to 30 minutes in the sun with
the face, arms, legs, or back exposed between 10 A.M. and 3 P.M. in the summer,
fall, and winter for just two days a week supplies all the vitamin D most
adults need (Robin, 2014, para. 3). The
body also stores vitamin D in the liver for 60 days. Nevertheless, the American Academy of
Dermatology warns against tanning (Robin, 2014, para. 4).
Beef liver, cheese, egg yolks, and omega-3 fatty fish all contain
relatively small amounts of vitamin D3 while mushrooms supply
vitamin D2. Cod liver oil,
however, is the best source of vitamin D other than the sun (Robin, 2014, para.
5). As for supplements, the Food and
Nutrition Board recommends a dose of 600 I.U. daily for everyone between one
and 70 and a dosage of 800 I.U. daily for adults over age 70 (Robin, 2014,
para. 6).
___________
Most multi-vitamins contain from 50 to
100 IU's of Vitamin D. The revised RDA for
vitamin D as of 2010 is 600 IU's from age 1 to 70 is 600 IU's, but at
age 71 it jumps up to 800 IU's. Even so, an adequate level of
vitamin D can be achieved from regular sun exposure on the face,
arms, and legs without sunscreen for between 15 to 30 minutes daily
(Mayo, 2016, para. 2).
However, to improve cognition, an
increase dosage of 528 to 9,000 IU's of Vitamin D2 or Vitamin D3 as
been taken daily by mouth from 8 to 40 weeks without harm (Mayo, 2016,
para. 9), so older adults with a fading memory and armed with this
blog page might wish to ask their physician about the advisablity of
upping their Vitamin D supplements. Of course, even though too much
sun causes sunburn, the body can't overdose on sun exposure from
Vitamin D. Nevertheless, the skin of older adults often has trouble
absorbing it.
Vitamin
D. Fact sheet for health professionals.
(2011 June 24). National Institutes of Health Office of Dietary Supplements. Table 3. Retrieved from http://ods.od.nih.gov/factsheets/VitaminD-HealthProfessional/
Selected
Food Sources of Vitamin D*
Cod liver oil (1 tablespoon): 1,360 I.U., 340 D.V.
Sockeye salmon (3 ounces): 447 I.U., 112 D.V.
Tuna, canned in water & drained (3 ounces): 154 I.U., 39 D.V.
Orange juice fortified with vitamin D (1 cup): 137 I.U., 34 D.V.
Fortified milk (1 cup): 115-124 I.U., 29-31 D.V
Fortified yogurt (6 ounces): 80 I.U., 20 D.V.
Sardines canned in oil & drained (2 sardines): 46 I.U., 12 D.V.
Beef liver cooked (3 ounces): 42 I.U., 11 D.V.
Egg (1 large): 41 I.U., 10 D.V.
Fortified ready-to-eat cereal: 40 I.U., 10 D.V.
Swiss cheese (1 ounce): 6 I.U. 2 D.V.
*BTW, i have removed margarine and sword fish
from this list because of recent medical findings: Medical research has connected the trans fats
in margarine to heart disease, and swordfish contains high levels of mercury.
 |
| Staying physically and mentally active should be everyone's goal. |
Taking a
brisk 20-minute walk outside after lunch, adding at least two servings of broiled or baked omega-3
fatty fish to the diet weekly, cultivating a taste for curries laced with
turmeric (curcumin), and taking vitamin D3 supplements just might
prevent or delay Mild Cognitive Impairment and Alzheimer’s. Moreover, since maintaining
an adequate supply of vitamin D also guards against the inflammation that causes
cardiovascular disease, it certainly will not hurt to take out this form of
long-term care insurance!
___________
Now for a personal note: Since I have written
and researched this blog page, I started taking 1,000 mg. of vitamin D daily
as well as taking a fish oil supplement that I had stopped taking in
the weeks before my mother died this spring. Some time later, I stopped this supplement, although I have continued to eat two servings of omega-3 fatty fish each
week. Consequently, I have noticed that my energy level has
increased even more than it usually does in the summer months even in the depths of an admittedly mild (compared to most places) Central Texas winter.
____________
The links furnished on this Web page represent the opinions of their authors, so they complement—not substitute—for a physician’s advice.