Meta-analysis
Proves Daily Habits Can Raise or Lower the Risk of Alzheimer’s
Evelyn
Smith
M.S.
in Library Science, University of North Texas (2012)
In the past week, many news sources have reported that
lifestyle choices made in early and in midlife directly or indirectly influence
whether individuals develop Alzheimer’s later in life. However, they all stem from the same source:
Xu, W., Tan, L., and Wang, H. F., et al. (2015, August
20). Meta-analysis of modifiable risk factors for Alzheimer's disease. Journal
of Neurology, Neurosurgery, and Psychiatry. pii: jnnp-2015-310548. doi: 10.1136/jnnp-2015-310548. [Epub ahead of
print]. [Abstract only]. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/26294005
Researchers affiliated with Qingdao University, in
Qingdao, China, and the University of California, San Francisco, evaluated the
association between Alzheimer’s and its modifiable risk factors by searching
the PubMed and Cochrane databases, identifying 323 article with 93 factors that
met their inclusion criteria for meta-analysis.
Xu, et al,
identified four pharmacological factors and four dietary factors that protected
users from Alzheimer’s. They also found a
biochemical exposure, homocysteine, and a psychological condition, depression, that
increase the risk of Alzheimer’s.
Meta-data showed how pre-existing diseases, like hypertension
and low-diastolic blood pressure as well as type 2 diabetes mellitus in
Asians—increase the risk for Alzheimer’s. Finally, lifestyle choices, such as
those evidenced by either a high body mass index (BMI) in midlife as well as
low BMI later in life intensify the probability of developing Alzheimer’s. However, cognitive activity, currently
smoking among Westerners, light-to-moderate drinking, stress, and high BMI late
in life decrease the risk of developing Alzheimer’s.
Conclusions:
Effective dietary and medical interventions, biochemical exposure,
psychological conditions, and pre-existing diseases and life styles may
decrease the risk for Alzheimer’s.
For an easy to follow review of these findings, Alice
Walton has summarized this meta-data analysis as follows:
Walton, Alice. (2015, August 22). The Lifestyle choices that affect Alzheimer’s
risk. Forbes. Retrieved from http://www.forbes.com/sites/alicegwalton/2015/08/22/the-lifestyle-choices-that-affect-alzheimers-risk/
University of California, San Francisco researchers
after surveying 323 studies on Alzheimer’s containing “high quality data” have
determined that most causes of Alzheimer’s are within each individual’s power
to avoid (Walton, 2015, August, 22, para. 1).
Protecting against Alzheimer’s are seven common sense
factors as well as links between medications and a reduced risk for
Alzheimer’s:
- Eating a healthy diet;
- Healthy intake of folate;
- Vitamin C, and vitamin E;
- Coffee consumption;
- Fish consumption;
- Light moderate drinking;
- Staying cognitively active;
- Estrogen;
- Cholesterol lowering drugs (statins);
- Blood pressure meds;
- Anti-inflammatory drugs (NSAIDs).
(Walton, 2015, August 22,
para. 2)
Surprisingly, exercise isn’t mentioned, even though it protects against some of the negative factors that researchers have coupled with a high risk of developing Alzheimer’s:
- Obesity;
- Depression;
- Carotid artery narrowing;
- Low educational attainment;
- High levels of homocysteine (a compound that builds up, in part when B vitamin levels are low);
- High blood pressure and low blood pressure;
- Frailty;
- Currently smoking (in Asians);*
- Type 2 diabetes (in Asians);*
(Walton, 2015, August 22,
para. 3)
Walton concludes that if everyone avoids these nine risk factors, this would cut the incidence of Alzheimer’s by two-thirds (Walton, 2015, August 22, para. 4).
*Read more about this advice, later. But for now, realize that smoking and Type 2 diabetes can raise the risk of dementia in all ethnic backgrounds.
| Now you know what to do, no excuses are acceptable! |
All of which leads to the following blog that fills in
some of the blanks:
____________
To-do
List of Ways to Avoid Alzheimer’s:
Eat
a healthy [Mediterranean, MIND, DASH, or traditional Asian] diet:
 |
| A heart-healthy diet and 30 minutes of aerobic exercise daily prevent & delay dementia. |
Diners can pick from several different style diet to
find delicious, heart and brain-healthy food that helps them prevent or delay
dementia:
Cohen, Paula. (2015, March 30). The MIND diet: 10 foods that fight
Alzheimer's (and 5 to avoid). CBS News. Retrieved from http://www.cbsnews.com/media/mind-diet-foods-avoid-alzheimers-boost-brain-health/
Martha Clare Morris and her fellow researchers at the
Rush University Medical Center in Chicago have developed the MIND diet,
claiming that faithfully following its tenets delays or prevents the risk of
dementia by 53 percent (Cohen, 2015, March 30, para. 2-4). Participants aged 58 to 98 in the Memory and
Aging Project filled out food questionnaires and underwent neurological testing
whereupon those that strictly followed its proposals upon testing had the
cognitive function of individuals 7.5 years younger than their chronological
age (Cohen, 2015, March 30, para. 5).
The MIND diet combines the Mediterranean and DASH diet
as well as emphasizing those foods, like blueberries, that have been proven
effective in fighting Alzheimer’s (Cohen, 2015, March 30, para. 7 & 13).
The MIND diet recommends six or more servings of green
leafy vegetables weekly, eating a green salad with at least one other vegetable
daily, adding some nuts to a diet five days a weekly, three servings of beans
or legumes weekly, three serving of whole grains daily, fish at least once
weekly, poultry twice weekly, cooking with olive oil, and a glass of red wine
daily (para. 19, Cohen, 2015, March 15, para. 9-18). It also limits red meat,
butter, and sweets, but not as severely as the Mediterranean diet does, and
allows cheese, fast food, and fried food to only once a week (Cohen, 2015,
March 15, para. 18).
Morris, M. C., Tangney, C. C., and Wang, Y., et al. (2015, June 15). MIND diet slows cognitive decline with
aging. Alzheimer’s & Dementia. (15)00194, 6S1552-5260. doi:
10.1016/j.jalz.2015.04.011. [Epub ahead of print]. [Abstract only]. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/26086182
Researchers tested the MIND diet, which emphasizes
neuro-protective components, finding it helped 960 participants in the Memory
and Aging Project lower their rate of cognitive decline over 4.7 years.
Mediterranean Diet—Topic overview. (2015). Heart Disease Health Center. WebMD. Retrieved from http://www.webmd.com/heart-disease/tc/mediterranean-diet-topic-overview
A Mediterranean diet features fish, fruit, vegetables,
beans, high fiber, whole grains, nuts, and olive oil while rationing meets,
cheese and sweets. Approximately 35 to 40
percent of all calories come from fish and olive oil and nuts (Mediterranean
Diet, 2015, para. 1-3).
What are the benefits? Adhering faithfully to a
Mediterranean diet might prevent heart disease, Type 2 diabetes, stroke,
Alzheimer’s depression, Parkinson’s disease, and metabolic syndrome
(Mediterranean Diet, 2015, para. 7).
How can you make the Mediterranean diet part of your
eating plan? Check out the foods that
are part of a Mediterranean diet and incorporate them in a personal diet plan
(Mediterranean Diet, 2015, para. 8).
- On the menu: Choose daily from a variety of fresh fruits and vegetables, whole-grains, unsaturated fats for mostly vegetarian meals, including Omega-3 fatty acid fish in meals at least twice weekly, but limiting poultry and eggs to only a few times a week and beef to only a few times a month and restricting sweets to only a few times a week (Mediterranean Diet, 2015, para. 9).
___________
Scarmeas, Nikolaos, Stern, Yakov, Tang, Ming Xin, et al.
(2006, June). Mediterranean diet and risk for Alzheimer’s disease. Annals
of Neurology. 59 (6), 912-921.
doi: 10.1002/ana.20854. [Full text]. Retrieved from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3024594/
After evaluating the diet of 2,258 cognitively healthy,
community-based New Yorkers and adjusting for cohort, age, gender, education,
apolipoprotein E genotype, caloric intake, smoking medical comorbidity, and
BMI, researchers concluded that strictly adhering to a Mediterranean diet
lowered the risk for Alzheimer’s disease (2006, June, Abstract, p. 912).
___________
Curinga, Karen. (2015). Why is an Asian diet more
healthy than an American diet? Live
Healthy. Houston Chronicle. Retrieved
from http://livehealthy.chron.com/asian-diet-healthy-american-diet-6022.html
Adopting a traditional Asian diet is a healthier way to
eat than the standard American diet (Curinga, 2015, para. 1):
- Higher Vegetable Consumption: Only 20 percent of an Asian diet’s calories come from meat (Curinga, 2015, para. 2).
- Healthier Cooking Techniques: Asian cooking uses low-fat cooking methods like stir-frying and steaming, substituting ginger, garlic, fresh herbs and chilis for salt while cooking foods quickly with very little oil (Curinga, 2015, para. 3).
- Less Red Meat Consumption: Asian cookery substitutes Omega-3 fatty fish, like tuna and salmon, for red meat—an option that reduces the risk for some cancers as well as heart disease. Tofu, a soybean product, also reduces cholesterol levels (Curinga, 2015, para. 4).
McCarron, Joshua. (2015, January 28). Asian diet to lose weight. Livestrong.
Retrieved from http://www.livestrong.com/article/316334-asian-diet-to-lose-weight/
- Features: Traditionally Asian diets avoid processed and refined foods, substitute green and black teas instead of sodas, and rely primarily on plant-based foods Consequently, Asian diets are higher in fiber than typical American diets but lower in calories (McCarron, 2015, January 28, para. 3).
- Typical Food: Steamed rice, vegetables, tofu and miso, fresh fish, eggs, and chicken make up the Asian diet (McCarron, 2015, January 28, para. 4).
- Asian Pyramid: Asians typically eat meat only about once a month while having a sweet, an egg, or some poultry only once a week. Daily components of the Asian diet are fish, shellfish, dairy products, vegetable oils, fruits, nuts, seeds, vegetables, legumes, and rice, noodles, and other grains (McCarron, 2015, January 28, para. 5).
- Considerations: Walking, stretching, and performing tai chi and taking part in the martial arts go along with an Asian diet (McCarron, 2015, January 28, para. 6).
___________
Stay
Active: Get in at least
two and a half hours of moderate aerobic exercise weekly.
| Both aerobic exercise & strength training build strong minds. |
Admittedly, this factor doesn’t appear on the list prepared
by Xu, et al, but a lack of daily exercise
does influence cardiovascular health, which, in turn, is a risk factor for
Alzheimer’s. It’s also the wise health
choice that busy working adults in midlife are most likely to skip. Indeed, 80
percent of all American adults don’t get enough exercise, although not doing so
leads to obesity and Type 2 diabetes, and exercise reduces the risk for
cardiovascular disease (Ryan, 2013, May 3, para. 2 & 6).
Ryan, Jason. (2013, May 3). CDC: 80 percent of American adults don’t get
recommended exercise. CBS News. Retrieved from http://www.cbsnews.com/news/cdc-80-percent-of-american-adults-dont-get-recommended-exercise/
__________
Ahlskog, J. E., Geda, Y. E., and Graff-Radford, N. R., et al. (2011, September). Physical exercise as a
preventive or disease-modifying treatment of dementia and brain aging. Mayo
Clinic Proceedings, 86(9), 876-84. doi: 10.4065/mcp.2011.0252. [Full text]. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/21878600
Using PubMed
keywords “exercise” and “cognition”, researchers looked for studies that
associated a reduced risk of dementia with midlife exercise. Meta-analysis confirmed that exercise in
middle age “significantly” reduced the risk of Mild Cognitive Impairment and
dementia. Moreover, in patients already diagnosed with dementia or MCI,
randomized controlled trials documented better cognitive scores in those who
participated in six to 12 months of aerobic exercise compared to their
sedentary controls, and one year of aerobic exercise in a large randomized
clinical trial of senior adults resulted in “significantly” larger hippocampal
volumes and improved spatial memory.
Similarly, animal studies show that exercise improves learning
outcomes. Aside from protecting the
neurons in the brain, physical exercise may also mitigate cerebrovascular risk.
Paillard, T. (2015). Preventive effects of regular
physical exercise against cognitive decline and the risk of dementia with age
advancement. Sports Medicine Open, 1(1):4. Epub 2015 April 17. [Full text]. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/26284161
Regular physical exercise increases the creation and
synthesis of neurotransmitters in the parts of the brain involved in thinking
and reasoning, and there is an inverse proportion between the amount of
physical activity and the risk of cognitive decline or the development of
neurodegenerative disease. The synthesis
of cerebral tissue under the influence of regular aerobic exercise possibly
increases the gray and white matter in the prefrontal and temporal cortex areas
as well as the volume of the hippocampus. Additionally, coordination exercise
stimulates cognitive function.
Petersen, Ronald. (2014, October 22). Can exercise prevent memory loss and improve
cognitive function? Diseases and Conditions:
Alzheimer’s Disease. Mayo Clinic. Retrieved from http://www.mayoclinic.org/diseases-conditions/alzheimers-disease/expert-answers/alzheimers-disease/faq-20057881
Possibly. Researchers
know that regular aerobic exercise reduces the risk of comorbidities for
Alzheimer’s like cardiovascular diseases and Type 2 diabetes while
strengthening bones and muscles and reducing stress, but studies also verify that
physically fit middle and older age adults are less likely to experience a
decline in mental performance (Petersen, 2014, October 22, para. 1-2).
Accordingly, aerobic exercise several times a week for
30 to 60 minute intervals may help healthy older adults retain their thinking
and reasoning skills; improve memory, reason, judgment and thinking skills for
those individuals diagnosed with Mild Cognitive Impairment and in the beginning
stages of Alzheimer’s; delay the onset of Alzheimer’s for individuals at risk
for developing dementia (Petersen, 2014, October 22, para. 3).
Physical exercise keeps an adequate supply of blood
flowing in the brain, but it also increases the chemicals that protect it,
counteracting the natural brain shrinkage that occurs with aging. More research is necessary to understand how
much physical activity improves memory or slows gradual cognitive decline, but
researchers do know that “regular exercise is important to stay physically and mentally fit” (Petersen, 2014,
October 22, para. 4-5).
__________
| Think dark green--as in leafy vegetables! |
Get enough folate
and Vitamin C and E
But put on hold on taking a Vitamin E supplement! By choosing a wise diet, most adults can receive their recommended daily allowance of folate, Vitamin C and E.
But put on hold on taking a Vitamin E supplement! By choosing a wise diet, most adults can receive their recommended daily allowance of folate, Vitamin C and E.
Folic acid in diet. (2015, August 3). Medline
Plus. US National Library of
Medicine. Retrieved from https://www.nlm.nih.gov/medlineplus/ency/article/002408.htm
Folate is found naturally in dark green leafy
vegetables, dried beans and peas, citrus fruits and juices, and enriched breads,
and cereals (Folic acid, 2015, August 3, para. 9-10).
___________
Morris, Martha Savaria. (2012, November). The role of B vitamins in preventing and
treating cognitive impairment and decline.
Advances in Nutrition. 3(6), 801-812. doi:
10.3945/an.112.002535. [Full
text]. Retrieved from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3648704/
Researchers extended the homocysteine theory of
cardiovascular disease to Alzheimer’s when they discovered a link between
vascular dementia and Alzheimer’s (Morris, 2012, November, Abstract, p. 801).
___________
Harrison, F. E. (2012).
A critical review of Vitamin C for the prevention of age-related
cognitive decline and Alzheimer’s disease. Journal
of Alzheimer’s Disease: JAD. 29 (4), 711-26. doi: 10.3233/JAD-2012-111853. [Full
text]. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/22366772
Maintaining a healthy Vitamin C level can protect
against age-related cognitive decline; moreover; deriving an adequate supply of
Vitamin C from diet is more
effective than taking supplements to
improve a diet low in Vitamin C (Harrison, 2012, Abstract, p. 711).
Zelman, Kathleen M. (2010, January 7). The benefits of Vitamin C. WebMD. Retrieved from http://www.webmd.com/diet/the-benefits-of-vitamin-c
Experts recommend taking a 500 milligram supplement of
Vitamin C daily to achieve health results on top of eating five serving of
fruits and vegetables since only 10 to 20 percent of all adults consume the
nine recommended servings of fruits and vegetables daily (Zelman, 2010, January
7, p. 1).
___________
Grimm, M. O., Stahlmann, C. P., and Mett, J., et al.
(2015, June). Vitamin E: Curse or
benefit in Alzheimer's Disease? A systematic investigation of the impact of α-,
γ- and δ-Tocopherol on Aß generation and degeneration in neuroblastoma cells. The Journal of Nutrition, Health and Aging.
19(6), 646-56. doi: 10.1007/s12603-015-0506-z. [Abstract only]. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/26054501
Although Vitamin E provides beneficial anti-oxidative
effect, as a tocopherol, it also has the potency to increase amyloid-β levels,
so researchers recommend that more studies are needed to find a form of Vitamin
E that can act both as an antioxidant and not increase beta amyloid plaque.
Whitbread, Daisy.
(2015). Top 10 foods highest in Vitamin E you can’t miss. HealthAliciousNess.com. Retrieved from http://www.healthaliciousness.com/articles/vitamin-E.php
- Tofu (Light, silken)
- Spinach (cooked)
- Nuts (almonds)
- Sunflower seeds (roasted)
- Avocados
- Shellfish (shrimp)
- Fish (Rainbow trout)
- Plant oil (Olive oil)
- Broccoli (cooked)
- Squash and pumpkins
___________
Lower high levels of homocysteine (which builds up when
Vitamin B levels are low):
| Fish, lean meat, poultry, egg, & dairy products all contain Vitamin B12. |
Fish, lean meat, poultry, and dairy and egg products and
fortified foods all are sources high in Vitamin B12 (Fear, 2015, January 18,
para. 4-9).
Fear, Georgie. (2015, January 18). List of foods high in Vitamin B12.
Livestrong. Retrieved from http://www.livestrong.com/article/25392-list-foods-high-vitamin-b12/
__________
Chen, H., Liu, S., and Ji, L., et al. (2015).
Associations between Alzheimer's disease and blood homocysteine, vitamin B12,
and folate: a case-control study. Current Alzheimer Research. 12(1):88-94.
[Abstract only]. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/25523421
Evaluating the association between Alzheimer’s and
levels of homocysteine (Hcy), Vitamin B12, and folate, Chinese researchers conducted a case study
that matched 115 patients with Alzheimer’s and 115 cognitively-health controls,
measuring their serum folate and Vitamin B12 using an automated immunoassay
analyzer, and measuring plasma Hcy with high-performance liquid
chromatography. They then analyzed the
link between Alzheimer’s and homocysteine, Vitamin B12 and folate, using binary
logistic regressions while adjusting for age and gender. Researchers correlated low vitamin B12 in
subjects with normal Hcy levels with Alzheimer's, high Hcy and low folate levels
with normal Vitamin B12 with Alzheimer’s, and high hcy levels, low vitamin B12
levels, and any folate level with Alzheimer’s. They concluded that a
combination of high Hcy, low Vitamin B12 and any folate level signified the weakest association with
Alzheimer’s.
Shen, L. and Ji, H. F. (2015, April 8). Associations between homocysteine, folic
acid, Vitamin B12 and Alzheimer's Disease: Insights from meta-analyses. Journal of Alzheimer’s Disease: JAD. [Epub
ahead of print]. [Abstact only]. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/25854931
Performing a search using Medline and Scopus databases,
using Stata 12.0 statistical software, a search identified 68 studies linking
homocysteine (Hcy), folic acid, and Vitamin B12 levels and Alzheimer’s. This meta-analysis associates Alzheimer’s
with higher levels of hcy and lower levels of folate acid and Vitamin B12 in
plasma than occurs in cognitively-healthy controls. Age-subgroup evaluation
also shows no age effect for hcy levels in plasma between Alzheimer’s patients
and controls, but it reveals that their
differences in folate and Vitamin B12 levels increase with age. Data additionally suggests that high hcy
levels and low folate levels correlate with an increased risk of Alzheimer’s.
___________
Daily drink three
cups of coffee:
| Enjoy coffee and tea without regret. |
Numerous studies suggest that caffeine may postpone the
onset of Alzheimer’s.
Mann, Denise. (2012, June 7). Drinking coffee may delay Alzheimer’s
disease. Alzheimer’s Disease Health
Center. WebMD. Retrieved from http://www.webmd.com/alzheimers/news/20120607/coffee-may-help-turn-tide-on-alzheimers-disease
Drinking three cups of coffee daily may slow the
progression of Alzheimer’s in older adults already starting to show signs of
memory loss. Starting at age 30, adults
should average drinking three eight-ounce cups of coffee daily (Mann, 2012,
June 7, p. 1).
Panza, P., Selfrizzi, V, and Barulli, M. R., et al. (2015, March). Coffee, tea and caffeine consumption and
prevention of late-life cognitive decline and dementia: A systematic review. The Journal of Nutrition, Health, & Aging. 19(3), 313-28. doi:
10.1007/s12603-014-0563-8. [Abstact only].
Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/25732217
Some case-controlled and cross-sectional and
longitudinal population-based studies provide evidence that coffee, tea, and
caffeine consumption may protect against late life cognitive decline. However longer, follow up studies are
necessary to establish a distinct dose response. Additionally, findings on whether caffeine
keeps Mild Cognitive Impairment from progressing to Alzheimer’s are too limited
to draw conclusions.
__________
Eat broiled, baked, or grilled [Omega 3, oily] fish
a minimum of at least once a week*:
| Substitute fish for beef as a diet's major protein source. |
*The Mayo Clinic and the American Heart Association,
however, call for eating fish twice a week (Mediterranean diet, 2015, p. 2; Omega 3 fatty acid, 2015, para. 21):
Mediterranean diet:
A heart-healthy lifestyle:
Nutrition and Healthy Eating.
Mayo Clinic. Retrieved from http://www.mayoclinic.org/healthy-lifestyle/nutrition-and-healthy-eating/in-depth/mediterranean-diet/art-20047801
Fish and Omega-3 fatty acid. (2015, June 15). American
Heart Association http://www.heart.org/HEARTORG/GettingHealthy/NutritionCenter/HealthyDietGoals/Fish-and-Omega-3-Fatty-Acids_UCM_303248_Article.jsp
___________
Addendum
August 31, 2015
However, please note that eating too much Omega-3 fish or overdoing fish or krill oil supplements
might have a disastrous effect:
Fish and Omega-3 fatty acid. (2015, June 15). American Heart Association. Retrieved from http://www.heart.org/HEARTORG/GettingHealthy/NutritionCenter/HealthyDietGoals/Fish-and-Omega-3-Fatty-Acids_UCM_303248_Article.jsp
Omega 3 fatty acids. (2015). University of Maryland Medical Center. Retrieved from http://umm.edu/health/medical/altmed/supplement/omega3-fatty-acids
The American Heart Association recommends that healthy
adults eat two servings of Omega-3 fatty
fish weekly, although the University of Maryland Medical Center cautions that
eating three servings of Omega-3 fish per week may raise the rise of hemorrhagic
stroke. The Website also warns that
it’s important to consult a physician before taking more than three grams of
Omega-3 fatty fish or krill oil capsules daily (Omega 3 fatty acid, 2015, para. 8 &
21).
__________
Cole, G. M. and Frautschy, S. A. (2010, April). DHA may
prevent age-related dementia. The Journal of Nutrition.
140 (4), 869-74. doi:
10.3945/jn.109.113910. Epub 2010 Feb 24.
[Full Text]. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/20181786
The risk of developing Alzheimer’s doubles every five
years after age 65—a statistic that necessitates a need for a “safe, effective
and affordable preventive” approach. Here
the (n-3 fatty acid docosahexaenoic acid (DHA) comes to the rescue since it
“appears to slow the onset of Alzheimer’s and possibly vascular dementia”: Clinical
trials hint that DHA or fish oil on its own can delay the early stages of
dementia, but larger trials are necessary to prove its effectiveness. DHA moderates some of the enzymes that slow
the division of tau-protein, increases brain levels of neuroprotective
brain-derived neurotrophic factor and reduces the (n-6) fatty acid arachidonate
as well as possibly helping suppress insulin/neurotrophic factor signaling
deficits, neuroinflammation, and oxidative damage that contribute to synaptic
loss and neuronal dysfunction in dementia (Cole, 2010, April, Abstract, p. 140).
Morris, Martha Clare, Evans, Dennis A., Bienias, Julia
L. (2003, July). Consumption of fish and
n-3 fatty acids and risk of incidence of Alzheimer’s Disease. JAMA Neurology. 60 (7), 940-46. doi:10.1001/archneur.60.7.940.http://archneur.jamanetwork.com/article.aspx?articleid=784412. [Full text].
Retrieved from http://archneur.jamanetwork.com/article.aspx?articleid=7844124
In a longitudinal study of Chicago-area older adults,
aged 65 to 94, from 1993 to 2000, researchers found that those who ate fish
once a week were 60 percent less likely to show signs of Alzheimer’s than those
who never or rarely ate fish (Morris, 2003, July, Abstract, p. 940).
Thomas, J., Thomas, C. J., and Radcliffe, J., et al. (2015). Biomed Research
International. 172801. doi: 10.1155/2015/172801. Epub 2015 Aug 2. Omega-3 fatty acids in early
prevention of inflammatory neurodegenerative disease: A focus on Alzheimer's
Disease. [Abstract only]. Retrieved from
http://www.ncbi.nlm.nih.gov/pubmed/26301243
Normal physiological changes of the brain caused by
aging include the depletion of long chain omega-3 fatty acids; moreover, the brains
of Alzheimer’s patients have lower docosahexaenoic acid (DHA) levels. Accordingly,
this study supports the role that long chain, Omega-3 fatty acids play in the
prevention or delay of cognitive decline in its earlier stages, although it
also calls for longer trials.
__________
Drink
a
glass of red wine daily:
| Drinking a glass of red wine protects against cardiovascular disease. |
Ma, T., Tan, M.S., and Yu, J. T., et al. (2014). Resveratol as a therapeutic agent for Alzheimer’s disease. BioMed Research International. doi: 10.1155/2014/350516. Epub 2014 Nov 26. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/25525597
Stay cognitively active:
Resveratol, a polyphenol found in red wine and many plants, displays neuro-protective properties, although its low bioavailability limits its effects.
Pasinetti, G. M. (2012, October). Novel role of red wine-derived polyphenols in the prevention of Alzheimer's disease dementia and brain pathology: experimental approaches and clinical implications. Planta Medica, 78(15): 1614-9. doi: 10.1055/s-0032-1315377. Epub 2012 Sep 21. [Full text]. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/23023952
Recent epidemiological and experimental evidence supports the hypothesis that grape-derived polyphenols interfere with the generation and assembly of β-amyloid peptides into neurotoxins, reducing tau accumulation (Pasinetti, 2012, October, Abstract, p. 1614).
___________
Stay cognitively active:
Continually challenging the mind keeps it sharp. Hence, storing up a cognitive reserve delays some of the effects of Alzheimer’s while also lessening the impact of beta amyloid plaque.
| Older adults can stay cognitively active all their lives. |
For individuals at risk for Alzheimer’s Occupational
Complexity (OCC) may confer resilience to the adverse effects of neuropathology
on cognition. 326 Middle-aged study
participants underwent a structural MRI, cognitive evaluation, and a work history
assessment.
Sobral, M.,
Pestana, M. H., and Paúl C. (2015, June).
Cognitive reserve and the severity of
Alzheimer's disease. Arquivos de Neuropsiquiatria.
73(6):480-6. doi: 10.1590/0004-282X20150044. [Full text]. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/26083882
Alzheimer’s patients with higher levels of Cognitive
Reserve, or the ability to cope with the effects of the neurodegenerative
process, are more likely to have a slower rate of cognitive decline, or so
researchers determined after examining two questionnaires, one of which
detailed their participation in leisure activities throughout life, filled out
by 75 outpatients diagnosed with probable Alzheimer’s (Sobral, 2015, June,
Abstract, p. 480).
Yang, Sarah. (2012, January 23). Lifelong
brain-stimulating habits linked to lower Alzheimer’s protein levels. Mind and Body. Berkeley
News. Retrieved from http://news.berkeley.edu/2012/01/23/engaged-brain-amyloid-alzheimers/
Yang and her fellow University of California, Berkeley
researchers have discovered that older adults who have taken part in
cognitively stimulating activities throughout their lives had fewer deposits of
beta-amyloid plaque than those who didn’t challenge themselves (Yang, 2012,
January 23, para. 1-2). Yang, et al asked 65 cognitively normal adults
age 60 and old how often they took part in “mentally engaging” activities from
age six to their present age. Researchers then gave the participants
neuro-psychological tests as well as PET scans, finding a “significant
association” between high levels of cognitive activity throughout a lifetime
and low levels of beta amyloid plaque (Yang, 2012, January 23, para. 10-11).
Yeung, S. T., Martinez-Coria, H., and Ager, R. R., et al.
(2015, July 7). Repeated cognitive stimulation alleviates memory
impairments in an Alzheimer’s disease mouse model. Brain Research Bulletin, 117, 10-15. doi:
10.1016/j.brainresbull.2015.07.001. [Epub ahead of print]. [Abstract only]. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/26162480
Researchers subjected 3xTg-AD mice to a “rigorous”
training routine starting at three months of age, consisting of training in a
new spatial recognition task in a Morris water maze every three months, ending
at 18 months of age. At this time, the
mice underwent testing in another hippocampus-dependent spatial task, using a
Barnes maze and in a cortical dependent novel object recognition memory task.
Data showed that periodic enrichment throughout the mice’s lives improved the
memory performance in aged 3xTg-AD mice when compared to “naïve aged matched
3xTg-AD mice”. Researchers noticed the effects of this “cognitive enrichment”
as early as six months of age. Thus,
they have hypothesized that “repeated cognitive enrichment can mitigate the
diverse cognitive deficits observed in Alzheimer's disease”.
___________
Take estrogen,
cholesterol-level drugs (statins), blood pressure medications, and
anti-inflammatory drugs (NSAIDs), or include natural sources of estrogen in
your diet:
DeMarco, Bob (2010, July 24). The estrogen dilemma and Alzheimer’s disease revisited. Alzheimer’s Reading Room. Retrieved from http://www.alzheimersreadingroom.com/2010/07/estrogen-dilemma-and-alzheimers-disease.html
Taking estrogen supplements might possibly guard against Alzheimer’s since researchers theorize that before menopause women are naturally protected against cognitive decline, but after menopause, they are at risk (DeMarco, 2010, para. 4). Indeed, 68 percent of all Alzheimer’s cases are women (DeMarco, 2010, para. 1).
Taking estrogen supplements might possibly guard against Alzheimer’s since researchers theorize that before menopause women are naturally protected against cognitive decline, but after menopause, they are at risk (DeMarco, 2010, para. 4). Indeed, 68 percent of all Alzheimer’s cases are women (DeMarco, 2010, para. 1).
14 foods that fight inflammation. (2015). Health Media Ventures. Retrieved from http://www.health.com/health/gallery/0,,20705881,00.html
Additionally, while foods high and sugar and saturated fats “spur” inflammation, some foods and herbs are naturally anti-inflammatory: fish, whole grains, dark leafy greens, nuts, soy, low fat dairy, peppers, tomatoes, beets, ginger and turmeric (or curcumin), garlic and onions, olive oil, beans, and tart cherries (14 foods, 2015),
Additionally, while foods high and sugar and saturated fats “spur” inflammation, some foods and herbs are naturally anti-inflammatory: fish, whole grains, dark leafy greens, nuts, soy, low fat dairy, peppers, tomatoes, beets, ginger and turmeric (or curcumin), garlic and onions, olive oil, beans, and tart cherries (14 foods, 2015),
____________________
Aim for a happy medium when improving blood pressure levels:
Blood pressure chart: What your reading means. (2015,
February 21). High Blood Pressure
(hypertension). Mayo Clinic. Retrieved from http://www.mayoclinic.org/diseases-conditions/high-blood-pressure/in-depth/blood-pressure/ART-20050982
Blood pressure that is too high or too low puts adults
at risk for brain damage:
High
Blood Pressure & Low Blood Pressure
Normal Blood Pressure:
Normal systolic blood pressure: Below 120
Normal diastolic blood pressure: Below 80
Prehypertension:
Systolic blood pressure: Between 120 and 139
Diastolic blood pressure: Between 80-89
High Blood pressure:
Systolic high blood pressure: 160 or higher
Diastolic high blood pressure: 100 or higher
| The DASH diet lowers blood pressure. |
________
Kruyer, A.,
Soplop, N., and Strickland S., et al. (2015, July).
Chronic hypertension leads to neurodegeneration in the TgSwDI mouse model
of Alzheimer's Disease. Hypertension.
66(10, 175-82. doi: 10.1161/HYPERTENSIONAHA.115.05524. Epub 2015 May 4.
[Abstract only]. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/25941345
“Hypertension, specifically, is an important modifiable
risk factor for late-onset Alzheimer’s” that researchers examined by chemically
inducing chronic hypertension in the TgSwDI mouse model of Alzheimer’s in early
adulthood, whereupon hypertension accelerated cognitive deficits in the Barnes
maze test a well as causing the deposits of microvascular deposits of β-amyloid
plaque and vascular inflammation. Moreover, hypertension causes hippocampal
neurodegeneration at an earlier age than normal in mice.
Meng, X. F., Yu, J. T., and Wang, H. F., et al. (2014). Midlife vascular risk
factors and the risk of Alzheimer's disease: A systematic review and
meta-analysis. Journal of Alzheimer’s
Disease. 42(4), 1295-310. doi: 10.3233/JAD-140954. [Abstract only]. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/25024338
In a systematic review and meta-analysis of published
cohort studies, researchers found “positive and significant” associations
between vascular risk factors, such as high blood pressure,
hypercholesterolemia, obesity, and diabetes mellitus in midlife and the
eventual risk of developing Alzheimer’s.
Norton, S., Matthews, F. E., and Barnes, D. E., et al. (2014, August; Erratum 2014,
November). Potential for primary
prevention of Alzheimer's disease: an analysis of population-based data. The Lancet: Neurology, 13 (8), 788-94;
Erratum (11), 1070. doi: 10.1016/S1474-4422(14)70136-X. [Abstract only]. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/25030513
Researchers estimated the population-attributable risk
of seven potentially modifiable risk factors for Alzheimer’s worldwide as well
as in the United States, the United Kingdom, and Europe: Diabetes, midlife
hypertension, midlife obesity, physical inactivity, depression, smoking, and
low educational attainment. The highest estimated PAR was for physical
inactivity in the US while all the risk factor PAR estimates were about 30
percent for the US, the UK, and Europe.
Assuming a causal relation and intervention at the appropriate age,
these seven risk factors could be reduced by 8.3 percent worldwide by 2050 by
improved access to education and targeting vascular risk factors for
improvement like physical activity, smoking, midlife hypertension and obesity,
diabetes, and depression.
10 ways to control high blood pressure without
medication. (2015, May 30). Diseases and
Conditions: High Blood Pressure
(Hypertension). Mayo Clinic. Retrieved
from http://www.mayoclinic.org/diseases-conditions/high-blood-pressure/in-depth/high-blood-pressure/art-20046974
- Loose extra pounds and watch your waistline: Loosing just ten pounds or 4.5 kilograms can reduce blood pressure. Generally, a man is at risk if his waist measures more than 40 inches, or 102 centimeters, while a woman is at risk if her waist measure more than 45 inches, or 89 centimeters (10 ways, 2015, May 30, para. 4-9).
- Exercise regularly: Exercising 30 minutes daily can lower blood pressure by 40 to 9 millimeters, but once someone stops exercising, his or her blood pressure goes up again. The Mayo Clinic suggests walking, jogging, cycling, swimming, and dances as the best ways to bring down blood pressure, although strength training can also reduce it (10 ways, 2015, May 30, para. 10-12).
- Eat a [heart-] healthy diet can lower blood pressure by 14 mm. Hg. The Mayo Clinic suggests keeping a food diary, boosting consumption of potassium, and shopping smart (10 ways, 2014, May 30, para. 12-17).
- Reduce sodium to bring down blood pressure by 2 to 8 mm. Hg., a task perhaps made more necessary for African Americans, adults over age 51, anyone already identified with high blood pressures, diabetes, or chronic kidney disease. This can be accomplished by reading food labels, eating less processed foods, not adding salt to dishes, and gradually reducing sodium intake (10 ways, 2014, May 30, para. 18-24).
- Limit alcohol intake: More than one drink daily in women and two drinks daily in men can raise blood pressure as well as reducing the effectiveness of blood pressure medication (10 ways, 2014, May 30, para. 25-27).
- Quit smoking: Stopping smoking helps blood pressure return to normal (10 ways, 2014, May 30, para. 28).
- Cut back on caffeine: To see if caffeine is raising one’s blood pressure, check it within 30 minutes of drinking a caffeinated beverage. Regularly drinking coffee only slightly raises blood pressure, however (10 ways, 2014, May 30, para. 29-31).
- Reduce stress: Chronic stress raised blood pressure, so the stressed out need to change their expectations, making plans to solve their problems that they can solve themselves, avoiding stress triggers, taking time out to relax, and being grateful for their blessings (10 ways, 2014, May 30, para. 32-39).
- Monitor blood pressure and regularly visiting a physician (10 ways, 2014, May 30, para. 40-41).
- Get support: Asking for and receiving support from family and friends as well as joining a support group can help bring down high blood pressure (10 ways, 2014,, May 30, para. 42-43).
__________
Steer Clear of Obesity: Exercise & diet away a high Body Mass
Index
| You are what you eat! |
Obesity in midlife increases the risk of Alzheimer’s in
late life, but a higher BMI in the elderly doesn’t necessarily increase the
risk for the older adults.
Anstey, K. J., Cherbuin, N., and Budge, M., et al. (2011, May). Body mass index in midlife and late-life as a
risk factor for dementia: A meta-analysis of prospective studies. Obesity
Reviews, 12(5), e426-37. doi:
10.1111/j.1467-789X.2010.00825.x. Epub 2011 Feb 23. [Abstract only]. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/21348917
A meta-analysis of 16 articles detailing the
relationship between Body Mass Index in mid and late life and dementia, evaluating
25,624 participants of Alzheimer’s, 15, 435 participants for vascular dementia,
and 30,470 participants for other types
of dementia, suggests either being underweight in midlife or overweight and
obese increases the risk of dementia.
______
Defining adult overweight and obesity. (n. d.). Division of Nutrition, Physical Activity, and
Obesity. Centers for Disease Control and
Prevention. Retrieved from http://www.cdc.gov/obesity/adult/defining.html
If BMI is 25.0 to 29.9, an individual is overweight; if
it is 30.0 or higher, he or she is obese (CDC, n. d., para. 3).
_________
Christensen, A. and Pike, C. J. (2015, July 7). Menopause,
obesity and inflammation: interactive risk factors for Alzheimer's disease. Frontiers in Aging
Neuroscience. 7, 130. doi: 10.3389/fnagi.2015.00130. eCollection 2015.
[Full-text]. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/26217222
The onset of menopause in women elevates their
vulnerability of Alzheimer’s disease, a risk associated with the depletion of
estrogen, increased central adiposity, and inflammation.
Naderali, Ebrahim, Ratcliffe, Stuart H., and Dale, Mark
C. (2009, October 2). Review:
Obesity and Alzheimer’s Disease: A link between body weight and cognitive
function in old age. American Journal of Alzheimer’s Disease and
Other Dementias. 24 (6), 445-449.
doi: 10.1177/1533317509348208. [Full text]. Retrieved from http://www.researchgate.net/profile/Ebrahim_Naderali/publication/26867791_Obesity_and_Alzheimer’s_disease_a_link_between_body_weight_and_cognitive_function_in_old_age/links/5411a7fb0cf264cee28b4bf4.pdf
Obesity’s role in cardiovascular disease and diabetes
may also contribute to the development of Alzheimer’s while obesity might also
impair glucose transport to the brain (Naderali, 2009, October 2, Abstract, p.
445).
Whitmer, R. A., Gustafson, D. R., and Barrett-Connor,
E. (2008, September). Central obesity
and increased risk of dementia more than three decades later. 30; 71(14):
1057-64. doi:
10.1212/01.wnl.0000306313.89165.ef. Epub 2008 Mar 26. [Abstract only]. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/18367704
A longitudinal analysis conducted on 6,583 Northern
Californians enrolled in Kaiser Permanente’s health plan had their sagittal
abdominal diameter measured from 1964 to 1973, and diagnoses of dementia in 15
percent of the patients occurred on average 36 years later from 1994 to
2006. After adjusting for age, gender,
race, education, marital status, diabetes, hypertension, hyperlipidemia,
stroke, heart disease, and medical utilization, compared with those patients
with the lowest quintile of SAD, those with the highest Body Mass Index were
the most likely to be diagnosed with dementia: 50 percent of those individuals
diagnosed with dementia in old age also were obese in the middle in midlife.
___________
Treat and prevent depression:
| It's important not to fight depression alone. |
Family members and friends should watch for signs of
depression in older adults particularly when they withdraw from others:
Baquero, M. and Martín, N. (2015, August). Depressive
symptoms in neurodegenerative diseases. World
Journal of Clinical Cases. 16; 3(8): 682-93. doi:
10.12998/wjcc.v3.i8.682. [Abstract
only]. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/26301229
Patients diagnosed with cognitive decline, whether they
suffer from Alzheimer’s, Parkinson’s, Lewy body dementia, vascular dementia, or
frontal temporal degeneration, exhibit the symptoms of depression at some point
during their presence. A large number of
patients are depressed during the early stages of neurologic disease without
clear evidence of neurological decline, although depressive symptoms can occur
later in neurodegenerative disease. In turn, depression further decreases
cognitive abilities and everyday functioning. Since depression is treatable,
their early detection is important in those individuals at risk for developing
dementia.
Qiu, W. Q., Zhu, H., and Dean, M., et al. (2015, August 6). Amyloid-associated depression and ApoE4
allele: longitudinal follow-up for the development of Alzheimer's disease. International Journal of Geriatric
Psychiatry. doi: 10.1002/gps.4339. [Epub ahead of print]. [Abstract only]. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/26250797
Qiu, et al
followed 223 cognitively-healthy older adults at baseline, giving them repeated
cognitive evaluations for the incident AD. Fifteen individuals, or seven
percent of the sampling, developed Alzheimer’s after an average follow-up time
of 6.2 years.
While no one with non-amyloid depression developed Alzheimer’s, nine percent of
the individuals diagnosed with amyloid-associated depression developed
Alzheimer’s. Additionally, ApoE4
carriers tended to have a much higher risk of developing Alzheimer’s than ApoE4
non-carriers (40% vs. 4%, p = 0.06). By way of contrast, eight percent of those
who did not have depression at baseline developed Alzheimer’s, but ApoE4 carriers and non-carriers
did not show a difference in Alzheimer’s
risk.
___________
Ease carotid artery narrowing:
| Are you at risk for cardiovascular disease? |
An inadequate blood supply to the brain causes
cognitive decline.
Claassen, J. A. (2015, May 15). New cardiovascular targets to prevent late
onset Alzheimer disease. European Journal
of Pharmacology. (15)00455-0, pii: S0014-2999doi:
10.1016/j.ejphar.2015.05.022. [Epub ahead of print]. [Abstract only]. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/25987416
Therapeutic strategies for reducing cardiovascular
disease may also reduce the incidence of dementia caused by Alzheimer’s
Disease. Longitudinal studies show a correlation between high blood pressure,
vascular stiffness, and the accumulation of beta amyloid plaque.
Hohman, T. J., Samuels, L. R., Liu D., et al. (2015, September). Stroke risk
interacts with Alzheimer's disease biomarkers on brain aging outcomes. Neurobiology of Aging. 36(9), 2501-8.
doi: 10.1016/j.neurobiolaging.2015.05.021. Epub 2015 Jun 6. [Abstract
only]. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/26119224
Although medical science has long known that
Alzheimer’s disease biomarkers and stroke risk factors have predicted cognitive
impairment independently, no researchers had evaluated the interaction between
stroke risk and AD markers on hippocampal volume and cognitive
performance. Consequently, researchers
analyzed data from the Alzheimer’s Disease Neuroimagining Initiative, autopsy
data from the National Alzheimer Coordinating Center, and stroke risk from the
Framingham Stroke Risk Profile. In the
first two studies, stroke risk interacted with tau and amyloid levels to
influence cognitive performance. However, stroke risk factors were greatest in
the absence of AD biomarkers or neuropathology, thus providing evidence that
Alzheimer’s Disease and stroke risk factors influence the ability to think and
reason independently.
Saito, S., Yamamoto, Y., and Ihara, M. (2015). Mild
Cognitive Impairment: At the crossroad of neurodegeneration and vascular
dysfunction. Current Alzheimer Research.
12(6):507-12. [Abstract only]. Retrieved
from http://www.ncbi.nlm.nih.gov/pubmed/26027811
Not only do most individuals diagnosed with Mild
Cognitive Impairment possess amyloid plaques and neurofibrillary tau tangles,
but at the same time, their cerebral vascular pathology shows signs of
arteriosclerosis and cerebral amyloid angiopathy (CAA). Because severe CAA is
an independent risk factor for dementia, clearing the brain of Aβ is a
potential treatment for both Alzheimer’s Disease and MCI. Moreover, controlling the risk factors for
both cardiovascular disease and dementia reduce the risk of MCI developing into Alzheimer’s.
___________
Upgrade the effects of low education:
 |
| It's never too late to learn new skills! |
Not only do years of schooling influence an older adult’s
risk for Alzheimer’s, but the quality of that schooling also influences whether
individuals experience cognitive decline.
Please note, however, that it’s never too late to learn new, challenging
skills, such as learning a foreign language or taking up Web design.
Chin, A. L., Negash, S., and Xie, S. (2012,
March). Quality, and not just quantity,
of education accounts for differences in psychometric performance between
African Americans and white non-Hispanics with Alzheimer’s disease. Journal of the International
Neuropsychological Society: JINS,
18(2):277-85. Doi: 10.1017/S1355617711001688. Epub 2012 Feb 3. [Full
text]. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/22300593
Chin, et al
examined the extent to which quality of education after controlling for years
of formal education accounted for the differences in cognitive performance in
African Americans and non-Hispanic, white Americans in 244 Alzheimer’s patients
who self-identified as either African American or white by using the Wechsler
Test of Adult Reading to estimate their quality of education. After controlling for age, gender, and years
of formal education, African Americans scored “significantly lower” than whites
on the Mini-Mental State Examination and on neuropsychological tests assessing
memory, attention, and language.
However, after adjusting for the patients’ reading levels, all differences
“significantly” diminished. Researchers
thus inferred that that quality, and not just quantity, of education” needs to
be considered when assessing cognitive performance in African Americans with
Alzheimer’s.
Mehta, K. M., Stewart, A. L., and Langa, K. M., et al. (2009, September). “Below
average” self-assessed school performance and Alzheimer’s disease in the Aging,
Demographics, and Memory Study. Alzheimer's and Dementia, 5(5): 380-7. Doi:
10.1016/j.jalz.2009.07.039. [Full text].
Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/19751917
Researchers examined whether a self-assessed
low-academic performance correlates with Alzheimer’s beyond the effects of the
Alzheimer’s patient’s education level when they asked 725 Aging, Demographics,
and Memory Study participants whether their academic
performance was above average, average, or below average: 11 percent of those with “above-average
performance had Alzheimer’s, 12 percent of the formerly average students had
Alzheimer’s, and 26 percent of the below average students had Alzheimer’s. After controlling for years in school, a
literacy test score, age, gender, race/ethnicity, apolipoprotein E-epsilon 4
status, socioeconomic status, and self-reported co-morbidity, those who regarded
themselves as “below average” academically were four times more likely to have
Alzheimer’s compared with those who were average. Accordingly, improving school performance in
addition to increasing the years of formal school may reduce the risk of
Alzheimer’s later in life.
P. S. -- As a semi-retired, former college English professor, I'd like to add that non-traditional older students from all ethnic and economic backgrounds were almost always my best--and most dedicated--students simply because they were more focused on their studies than the average 18 to 21-year-old even while working, keeping up their family responsibilities, and going to school. So don't be afraid to go back to school at any age. You may be pleasantly surprised!
P. S. -- As a semi-retired, former college English professor, I'd like to add that non-traditional older students from all ethnic and economic backgrounds were almost always my best--and most dedicated--students simply because they were more focused on their studies than the average 18 to 21-year-old even while working, keeping up their family responsibilities, and going to school. So don't be afraid to go back to school at any age. You may be pleasantly surprised!
__________
Prevent frailty’s
effect upon cognitive ability:
| Old age doesn't necessary correlate with frailty. |
Addendum
August 28, 2015
Morley, John E., Morris, John C. Berg-Weger, Marla, et al. (2015, September 1). Brain Health: The Importance of Recognizing Cognitive Impairment: An IAGG Consensus Conference. Journal of Post-Acute and Long-term Care Medicine. 16(9), 731-739. doi: http://dx.doi.org/10.1016/j.jamda.2015.06.017 [Abstract only]. Retrieved from http://www.jamda.com/article/S1525-8610%2815%2900438-7/abstract
Early diagnosis of cognitive decline is a right owed every mentally-impaired older adult. Moreover, recognizing early symptoms of Mild Cognitive Impairment allows for appropriate diagnosis and treatment that also allows for individual to participate in the decision-making process about his or her future: Additionally, 1) screening tests take only three to seven minutes to administer; 2) consultation with both individual and family member or friends who suspect that his or her cognitive powers are declining is an appropriate approach to take; 3) MCI may have treatable aspects, and 4) a combination of medical and lifestyle interventions may delay or prevent cognitive decline.
Bottom
Line: At the first
sign of mental impairment, schedule an appointment for your loved one with a
neurologist. Preventive actions taken
when older adults are first diagnosed with Mild Cognitive Impairment may prevent or
delay Alzheimer's. Also, during this stage of cognitive decline, the MCI
patient and his or her family can make financial planning decisions and living
arrangements together should he or she eventually be diagnosed with
Alzheimer's. Remember, Mom, Dad, or Aunt Susie is still an adult and deserves to be treated like one!
___________
Buchman, A. S., Boyle, Patricia, A., Wilson, Robert
S. (2007, June). Frailty is associated with incident
Alzheimer’s disease and cognitive decline in the elderly. Psychosomatic
Medicine. 69, 483-489. doi:
10.1097/psy.0b013e318068de1d. [Full
Text]. Retrieved from http://www.researchgate.net/profile/Patricia_Boyle3/publication/6279551_Frailty_is_associated_with_incident_Alzheimer's_disease_and_cognitive_decline_in_the_elderly/links/0c96052853de735245000000.pdf
In a longitudinal study of 823 elderly conducted by the
Rush Memory and Aging Project analyzing possible links between frailty,
cognition, and Alzheimer’s, both at baseline and annually, frailty correlated
with an increased risk of incident Alzheimer’s (Buchman, 2007, June, Abstract,
483).
Canevelli, M., Cesari, M., and Van Kan, G. A. (2014,
January). Frailty and cognitive decline:
how do they relate? Current Opinion in Clinical Nutrition and Metabolic Care. 18(1),
43-50. doi: 10.1097/MCO.0000000000000133. [Abstract only]. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/25405314
Physical frailty predicts the incidence of cognitive
impairment and dementia in longitudinal studies while cross-sectional studies
indicate that the frail elderly have a lower cognitive performance than their
non-frail peers. Even so, randomized, controlled
trials are necessary for treatment to improve the cognitive abilities of older
patients in poor health.
__________
The next two factors supposedly apply only to Asians,
although the Centers for Disease Control notes that smoking contributes to
cardiovascular disease (CDC, 2014, para. 3), which, in turn, contributes to the
risk for developing Alzheimer’s, and
Swedish researchers have determined that prediabetes increases one’s
risk of Alzheimer’s by 70 percent (Mann, 2006, para. 7).
Mann, Denise. (2006, July 17). Diabetes: New links to Alzheimer’s. Diabetes Health Center. WebMD.
Retrieved from http://www.webmd.com/diabetes/news/20060717/diabetes-link-alzheimers
Smoking & tobacco use. (2014, February 6). CDCL
Centers for Disease Control and Prevention. Retrieved from http://www.cdc.gov/tobacco/data_statistics/fact_sheets/health_effects/effects_cig_smoking/index.htm
___________
Stop [or never taking up] smoking (among Asians):
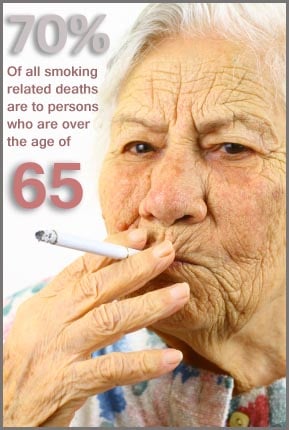 |
Why the researchers listed smoking as a poor lifestyle
choice specifically for Asians* rather than for everyone on Earth must have
gotten lost in translation since smoking is linked to chronic heart and
cardiovascular disease (Smoking, 2013, para. 5).
List of smoking-related diseases expanded. (2013). NBC News.
Associated Press. Retrieved from http://www.nbcnews.com/id/5077308/ns/health-addictions/t/list-smoking-related-diseases-expanded/
___________
Cho, H., Kim, C.,
Kim, H. J. (2015, August 11). Impact of smoking on neuro-degeneration and
cerebrovascular disease markers in cognitively normal men. European
Journal of Neurology. doi:
10.1111/ene.12816. [Epub ahead of print]. [Abstract only]. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/26264353
Korean researchers surveyed the results after 977
cognitively normal men received medical check-ups, including a 3.0T magnetic
resonance imaging at a health promotion center, and the results placed them in
the following categories: Never smoked, smoked in the past, and current
smokers. Current smokers exhibited a
cortical thinning in their frontal and temporo-parietal lobes when compared
with those men who had never smoked. However, no links existed between smoking
and the severity of white matter hyper-intensity or in the number of
lacunes. Researchers therefore concluded
that smoke might influence neuro-degeneration in cognitively health man rather
than worsening their cerebrovascular health. They then inferred that the impact
of smoking on Alzheimer’s might be modifiable.
Durazzo, T. C., Meyerhoff, D. J., and Mon, A. et al. (2015, April 9). Chronic cigarette smoking in healthy
middle-aged individuals is associated with decreased regional brain n-acetylaspartate
and glutamate levels. Biological Psychiatry. (15), 00283-8. pii:
S0006-3223. doi:
10.1016/j.biopsych.2015.03.029. [Epub ahead of print]. [Abstract only]. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/25979621
Chronic smoking in young and middle-aged individuals correlates
with “significant age-related neurobiological abnormalities” in the brain’s
anterior frontal regions linked to the development and maintenance of addictive
disorders. After comparing N-acetylaspartate
(NAA), choline-containing compounds, creatine-containing compounds (Cr),
myo-inositol (mI), and glutamate (Glu) levels in the anterior cingulate cortex
and the right dorsolateral prefrontal cortex of young and middle-aged smokers
and nonsmokers using 4-tesla proton single volume magnetic resonance
spectroscopy, researchers examined their decision-making, risk taking, and
self-reported impulsivity. The smokers
exhibited lower DLPFC, NAA, Cr, mI and Glu concentrations than their
non-smoking peers. They also showed poor
decision-making skills and greater impulsivity.
_________
Prevent Type 2 diabetes (among Asians):
Again, it’s a mystery why researchers singled out Asians*
as being particularly at risk if they have diabetes. After all, anyone with Type 2 diabetes is at
greater risk for heart attack and stroke (Complications, 2015, January, para.
2).
What complications (problems) care caused by
diabetes. Department of Health. New York State. Retrieved from http://www.health.ny.gov/diseases/conditions/diabetes/problems_caused_by_diabetes.htm
___________
Sridhar, G. R., Lakshmi, G., and Nagamani, G. (2015,
June 10). Emerging links between type 2 diabetes and Alzheimer's disease. World
Journal of Diabetes. 6(5), 744-51.
doi: 10.4239/wjd.v6.i5.744.
[Full-text]. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/26069723
Indian researchers emphasize that epidemiological,
clinical, biochemical, and imaging studies link Type 2 diabetes mellitus and
Alzheimer's disease with increasing age and note that being diagnosed with
either disease increases the risk of developing the other. While cross sectional studies undoubtedly confirm
this association, cross sectional studies, however, reveal the many complex
ways diabetes and Alzheimer’s interact with each other. Additionally, Sridhar, et al recognize that they share certain life style risk factors,
such as obesity, dyslipidemia, insulin resistance and sedentary habits, as well
as certain pathogenic factors, so lifestyle changes and pharmacological agents should
be able to prevent or delay their develpment. Paradoxically, not only do life style choices
protect against Alzheimer’s disease, but the drugs used in the treatment of
diabetes, such as intranasally-delivered insulin, also guard against dementia. Furthermore, since a Type 2 diabetes is a
recognized risk factor for Alzheimer’s, clinicians must take the responsibility
for preventing or postponing Alzheimer’s after a Type 2 diabetes diagnosis.
Zhang, Z., Fang, P., and Shi, M., et al. (2015, August 4). Elevated galanin may predict the risk of
type 2 diabetes mellitus for development of Alzheimer's disease. Mechanisms
of Ageing and Development. 150, 20-26. doi: 10.1016/j.mad.2015.08.001.
[Epub ahead of print]. [Abstract only].
Developing evidence indicates that galanin defects perform
a central role in type 2 diabetes mellitus, a risk factor for Alzheimer’s. Current
data also supports the hypothesis that activating central GalR2 weakens insulin
resistance in animal models.
The study finds a correlation between these factors and
Alzheimer’s; however, it doesn’t prove that any one of them directly causes
Alzheimer’s (Walton, 2015, August 22, para. 3-4).
___________
The links
furnished on this Web page represent the opinions of their authors, so
they complement—not substitute—for a physician’s advice.
_____________
Mayo
Clinic Publicizes Tests for Alzheimer's
Petersen,
Ronald. (2015). Alzheimer's test: Detection at the earliest stages.
Mayo Clinic. Retrieved from
https://www.mayoclinic.org/diseases-conditions/alzheimers-disease/expert-answers/alzheimers-test/faq-20057850
New Alzheimer's tests, not yet widely available, detect the pathological components of Alzheimer's:
- Biomarker Test: Assessment examines the spread of beta-amyloid patterns within the brain;
- Brain Imaging (neuroimaging): Procedure records changes within the brain;
- Cognitive Assessment: Computer-based assessment may detect early cognitive changes.
Early
detection allow for intervention with medication that slows the
advance of Alzheimer's.
No comments:
Post a Comment